·Clinical Research··Current Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO·
Relationship between dacryoadenitis subtype of idiopathic
orbital inflammatory pseudotumor and paranasal sinusitis
Jing Li, Xin Ge, Jian-Min Ma
Beijing Tongren Eye Center, Beijing Tongren Hospital, Capital Medical
University, Beijing Ophthalmology and Visual Sciences Key Laboratory, Beijing
100730, China
Correspondence to: Jian-Min
Ma. Beijing Tongren Eye Center, Beijing Tongren Hospital, Capital Medical
University, Beijing Ophthalmology and Visual Sciences Key Laboratory, No. 1
Dongjiaominxiang Street, Dongcheng District, Beijing 100730, China.
jmma@sina.com
Received: 2014-12-03 Accepted:
2015-06-08
Abstract
AIM: To determine the clinical features of the dacryoadenitis subtype
of idiopathic orbital inflammatory pseudotumor and its relationship with
paranasal sinusitis.
METHODS: A retrospective analysis of 46 patients who
received surgical treatment at the Department of Ophthalmology, Beijing Tongren
Hospital, Capital Medical University for the dacryoadenitis subtype of
idiopathic orbital inflammatory pseudotumor from October 2010 to December 2012.
Each patient underwent magnetic resonance imaging (MRI) of the orbits and the 4
paranasal sinuses. Disease status and the level of serum immunoglobulin G4
(IgG4) was measured before and 6mo after surgery.
RESULTS: The initial clinical feature of the idiopathic
dacryoadenitis type of orbital inflammatory pseudotumor was redness or swelling
of the eyelids. Masses were palpated in the area of the lacrimal gland in some
patients. Of the 46 patients, 16 also suffered from sinusitis (34.8%), with 14
cases of ethmoid sinusitis, 8 cases of maxillary sinusitis, 9 cases of sphenoid
sinusitis, and 8 cases of frontal sinusitis. Of the 16 patients with sinusitis,
4 patients had a medical history of rhinitis (range: 10mo to 15y previously),
10 patients had occasional nasal congestion, and 2 patients had no nasal
congestion. Thirteen of the 46 patients had elevated serum IgG4 levels. Nine of
these 13 patients had MRI signs of sinusitis. All patients (n=46) received oral glucocorticoid
treatment for approximately 3mo after surgery. No sign of recurrence was found
in the orbital MRI 6mo after surgery. Of the 16 patients with sinusitis, 9
cases of elevated serum IgG4 levels improved after treatment with decreased
serum IgG4 level and 7 cases of normal serum IgG4 levels remained unchanged.
CONCLUSION: Some patients with the dacryoadenitis subtype of
idiopathic orbital inflammatory pseudotumor may also suffer from paranasal
sinusitis. The incidence of paranasal sinusitis was much higher in patients
with IgG4-elevated dacryoadenitis subtype orbital inflammatory pseudotumor than
in those with normal IgG4 levels. Dacryoadenitis subtype orbital inflammatory pseudotumor and paranasal
sinusitis may both the clinical manifestations of IgG4-related disease involved
in different locations.
KEYWORDS: orbital disease; inflammatory pseudotumor;
sinusitis; immunoglobulin G4
Citation: Li J, Ge X, Ma JM.
Relationship between dacryoadenitis subtype of idiopathic orbital inflammatory
pseudotumor and paranasal sinusitis. Int
J Ophthalmol 2016;9(3):444-447
INTRODUCTION
Idiopathic orbital inflammatory pseudotumor (IOIP) is a common orbital
disease which severely affects human health. The incidence of IOIP is second
only to thyroid-associated ophthalmopathy and lymphoproliferative disorders.
IOIP accounts for 7.1% of orbital diseases[1-4]. Clinical manifestations can
affect various orbital structures including the lacrimal glands, extraocular
muscles, and orbital fat[5]. Since histopathologic findings in IOIP are not
specific, the diagnosis of this disease is mainly based on the exclusion of
other causes of the symptoms (e.g.
cancer, infections, and other specific inflammations[5]). Further
research of the etiology and pathogenesis of IOIP is needed to improve our
fundamental understanding of the disease and facilitate diagnosis and
treatment.
Recent studies[6-10]
have suggested a possible relationship between IOIP and sinusitis. Yan et al[11] reported that 36 of 209
(17.2%) cases of sinusitis were accompanied by orbital inflammatory
pseudotumor. IOIP can be classified into different subtypes based
on the involved structures: dacryoadenitis, myositis, optic perineuritis, or
diffuse inflammation subtypes. However, all the above researches didn’t measure
the level of serum immunoglobulin G4 (IgG4).
Thus, this study analyzed the relationship between the dacryoadenitis subtype of IOIP and sinusitis and investigated the
relationship with IgG4.
SUBJECTS AND
METHODS
Subjects This study was approved by the ethics committee of Beijing Tongren
Hospital, and informed consent was obtained from each patient in accordance
with the Declaration of Helsinki. Forty-six patients with the dacryoadenitis subtype
of IOIP that received treatment at the
Department of Ophthalmology, Beijing Tongren Hospital, Capital Medical
University between October 2010 and December 2012 were evaluated. All patients had their diagnosis confirmed by
post-operative histopathologic exam. Benign lymphoepithelial lesions of the
lacrimal gland, lymphoma, thyroid-associated ophthalmopathy, and other diseases with similar clinical manifestations
as the dacryoadenitis subtype of IOIP were
excluded.
Methods After histopathological confirmation of the dacryoadenitis subtype of IOIP,
magnetic resonance imaging (MRI) of each patient’s orbits was performed to
evaluate the 4 pairs of paranasal sinuses. MRI and serum IgG4 were both
performed 6mo after surgery to identify recurrence of dacryoadenitis and
improvement of any paranasal sinusitis.
RESULTS
Clinical Features Sixteen of 46
patients with the dacryoadenitis subtype of IOIP had sinusitis. Among these 16
patients there were 13 males and 3 females with a median age of 42y (range:
11-69y). Seven cases involved the right eye, 2 the left eye, and 7 both eyes.
The course of disease ranged from 1 to 62mo. Initial manifestations included
redness or swelling of the eyelids. Soft masses were palpable in the lacrimal
gland of 8 patients.
Cases Combined with Sinusitis Sixteen of the 46 patients in this study had
sinusitis (34.8%), with 14 cases of ethmoid sinusitis, 8 of maxillary
sinusitis, 9 of sphenoid sinusitis, and 8 of frontal sinusitis. Of the 16
patients with sinusitis, 4 patients had a medical history of rhinitis (range:
10mo to 15y previously), 10 had occasional nasal congestion, and 2 had no nasal
congestion. Among the patients with sinusitis, 5 patients had inflammation in 1
group of sinuses, 4 had inflammation in 2 groups of sinuses, 2 had inflammation
in 3 groups of sinuses, and 5 had inflammation in 4 groups of sinuses.
Relationship Between Serum IgG4 Levels and Idiopathic
Orbital Inflammatory Pseudotumor and Sinusitis Thirteen of the 46 patients had elevated serum IgG4
levels. Nine of these 13 patients had MRI signs of sinusitis (Figure 1 and
Table 1).
Table 1 General clinical data of 16 both
dacryoadenitis subtype of IOIP and sinusitis patients
|
Patient no. |
Age (a) |
Sex |
Duration (mo) |
Eye involved |
Sinus included |
IgG4 level (mg/dL) |
Follow-up status |
|
1 |
69 |
M |
26 |
R |
ALL |
515 |
|
|
2 |
17 |
M |
28 |
L |
LE |
160 |
Improve |
|
3 |
0 |
M |
36 |
B |
BS |
472 |
Improve |
|
4 |
42 |
M |
3 |
B |
BE+BM+BS |
136 |
Improve |
|
5 |
48 |
M |
60 |
B |
LF+BE |
1350 |
Improve |
|
6 |
28 |
M |
10 |
B |
BF+BE+SM |
1250 |
Improve |
|
7 |
11 |
M |
62 |
L |
RS |
740 |
Improve |
|
8 |
43 |
M |
37 |
B |
ALL |
1800 |
Improve |
|
9 |
60 |
M |
25 |
B |
ALL |
1601 |
Improve |
|
10 |
37 |
F |
12 |
R |
ALL |
<7.4 |
No obvious improve |
|
11 |
42 |
M |
12 |
B |
BE+LM |
24.2 |
No obvious improve |
|
12 |
41 |
F |
3 |
R |
RE |
<7.4 |
No obvious improve |
|
13 |
22 |
M |
2 |
R |
BE+RS |
20.7 |
No obvious improve |
|
14 |
67 |
M |
1 |
R |
BF+BE |
68.8 |
No obvious improve |
|
15 |
38 |
F |
9 |
R |
ALL |
<7.4 |
No obvious improve |
|
16 |
58 |
M |
38 |
R |
LE |
74.2 |
No obvious improve |
M: Male; F:
Female; L: Left; R: Right; B: Both eyes; E: Ethmoiditis; S: Sphenoiditis; M:
Maxillary sinusitis; F: Frontal sinusitis.
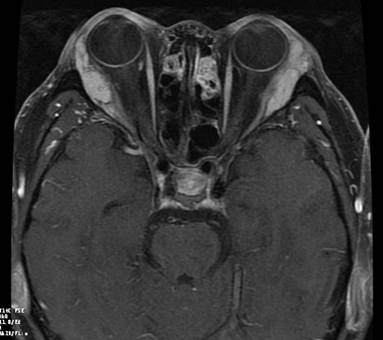
Figure 1 A IOIP patients had MRI signs of sinusitis.
Follow-up Cases All patients (n=46) in this
study received oral glucocorticoid treatment for approximately 3mo after
surgery. No sign of recurrence was found in all patients on the 6mo
post-operative MRI. Of the 16 patients with sinusitis, 9 cases with elevated
serum IgG4 levels had a decrease in these levels after treatment and 7 cases
with normal serum IgG levels had no change in these levels.
DISCUSSION
IOIP is a non-specific orbital inflammation that
may occur in any age group, although it is more common in the elderly. Both
genders are equally affected. IOIP may occur unilaterally, in both eyes
simultaneously, or sequentially in both eyes[1-4]. Correlation studies
between IOIP and sinusitis have been reported as early as the 1980s. The
conclusion of each study varied, but most showed a correlation between the two
diseases. In 1980, Fortson et al[6] first
reported 5 cases of IOIP invading the maxillary sinus. In 1981, Eshaghian and
Anderson[7]
reported 2 IOIP cases with a recent history of sinusitis. Few studies have
shown no correlation between the two diseases. In our study, a total of 46
cases of the dacryoadenitis subtype of IOIP were treated, and 16 patients had
sinusitis. The frequency of co-existing sinusitis in our patients was higher
than in previous reports. This higher rate may be due to ineffective previous
treatment at other hospitals, the severe condition, and long medical history.
Previous reports have not classified the subtypes of IOIP. To improve the
comparability and objectivity of our findings, we only studied the
dacryoadenitis subtype of IOIP. Our results suggest that the dacryoadenitis
subtype of IOIP is associated with paranasal sinusitis at a higher rate than in
previous reports[6-11]. Further research will be necessary to determine the reason. Most
patients we treated had no obvious symptoms of sinusitis, even though the
imaging tests were compatible with sinusitis.
The spectrum of
IgG4-related diseases (IgG4-RD) has been expanding since the first report of
autoimmune pancreatitis by Hamano et al[12] in 2001.
To date, the diagnostic criteria of IgG4-RDs have not been unified, but
elevated IgG4 serology or the presence of numerous IgG4-positive plasma cells
suggests their involvement in the pathogenesis of autoimmune diseases[13-20].
Thirteen of the 46 patients in this study had elevated serum IgG4 levels,
suggesting that some dacryoadenitis
subtypes of IOIP belong to the category of IgG4-RDs. A correlation between
IgG4-IOIP and paranasal sinusitis has not been previously reported. Among the
13 patients with the dacryoadenitis subtype of IOIP and elevated serum IgG4, 9
had MRI findings of sinusitis and these patients had significantly higher IgG4
levels than patients with sinusitis alone, suggesting that IgG4 may play an
important role in sinus and orbital disease.
Treatment of IOIP consists of symptomatic
treatment, radiotherapy, and surgery. Glucocorticoids are widely recognized as
the preferred treatment[1-2]. All patients in this study received oral
glucocorticoids for approximately 3mo after surgery. No sign of recurrence was
found in any patient on the 6mo post-operative MRI. Of the 16 patients with
sinusitis, 9 improved after treatment and 7 had no significant change in
symptoms. Patients that improved after treatment had high serum IgG4 levels
before surgery, suggesting the presence of an IgG4-RD subtype. Thus,
glucocorticoids effectively controlled orbital and sinus inflammatory lesions
in patients with IgG4-RD.
In summary, this study
showed a close relationship between the dacryoadenitis subtype of IOIP and sinusitis. The frequency of sinusitis
in patients with the IgG4-elevated dacryoadenitis subtype of IOIP was
significantly higher than that in patients with normal serum IgG4 levels. A
possible explanation is the close anatomic relationship between each group of
paranasal sinuses and the orbital cavity. Further research is necessary to
confirm this hypothesis. Dacryoadenitis subtype of idiopathic orbital
inflammatory pseudotumor and paranasal sinusitis may both the clinical
manifestations of IgG4-related disease involved in different locations.
ACKNOWLEDGEMENTS
Foundation:
Supported by the National Natural Science Foundation of China (No. 81371052).
The funders had no role in study design, data collection and analysis,
decision to publish, or preparation of the manuscript.
Conflicts of Interest: Li J, None; Ge X, None; Ma JM, None.
REFERENCES
1 Espinoza GM. Orbital inflammatory pseudotumors:
etiology, differential diagnosis, and management. <ii>Curr Rheumatol
Rep</ii> 2010;12(6):443-447. [CrossRef] [PubMed]
2 Pemberton JD, Fay A.
Idiopathic sclerosing orbital inflammation: a review of demographics, clinical
presentation, imaging, pathology, treatment, and outcome. <ii>Ophthal
Plast Reconstr Surg</ii> 2012;28(1):79-83. [CrossRef] [PubMed]
3 Berry-Brincat A, Rose GE.
Idiopathic orbital inflammation: a new dimension with the discovery of
immunoglobulin G4-related disease. <ii>Curr Opin Ophthalmol</ii>
2012;23(5):415-419. [CrossRef]
[PubMed]
4 Szabo B, Szabo I, Crisan D,
Stefanut C. Idiopathic orbital inflammatory pseudotumor: case report and review
of the literature. <ii>Rom J Morphol Embryol</ii>
2011;52(3):927-930. [PubMed]
5 Pakdaman MN, Sepahdari AR,
Elkhamary SM. Orbital inflammatory disease: Pictorial review and differential
diagnosis. <ii>World J Radiol</ii> 2014;6(4):106-115. [CrossRef] [PubMed] [PMC free article]
6 Fortson JK, Shapshay SM,
Weiter JJ, Vaughan CW, Strong MS. Otolaryngologic manifestations of orbital
pseudotumors. <ii>Otolaryngol Head Neck Surg</ii>
1980;88(4):342-348. [PubMed]
7 Eshaghian J, Anderson RL.
Sinus involvement in inflammatory orbital pseudotumor. <ii>Arch
Ophthalmol</ii> 1981;99(4):627-630. [CrossRef]
[PubMed]
8 Heersink B, Rodrigues MR,
Flanagan JC. Inflammatory pseudotumor of the orbit. <ii>Ann
Ophthalmol</ii> 1977;9(1):17-22, 25-29. [PubMed]
9 Leibovitch I, Goldberg RA,
Selva D. Paranasal sinus inflammation and non-specific orbital inflammatory
syndrome: an uncommon association. <ii>Graefes Arch Clin Exp
Ophthalmol</ii> 2006;244(11):1391-1397. [CrossRef] [PubMed]
10 Mahr MA, Salomao DR, Garrity
JA. Inflammatory orbital pseudotumor with extension beyond the orbit.
<ii>Am J Ophthalmol </ii>2004;138(3):396-400. [CrossRef] [PubMed]
11 Yan J, Wu Z, Li Y. 36 case
idiopathic orbital inflammatory pseudotumor with sinus involvement.
<ii>Lin Chuang Er Bi Yan Hou Ke Za Zhi</ii> 2002;16(8):410-411. [PubMed]
12 Hamano H, Kawa S, Horiuchi
A, <ii>et al</ii>. High serum IgG4 concentrations in patients with
sclerosing pancreatitis. <ii>N Engl J Med</ii>
2001;344(10):732-738. [CrossRef]
[PubMed]
13 Umehara H, Okazaki K, Masaki
Y, <ii>et al.</ii> Comprehensive diagnostic criteria for
IgG4-related disease (IgG4-RD), 2011. <ii>Mod Rheumatol</ii>
2012;22(1):21-30. [CrossRef]
14 Wallace ZS, Stone JH. An
update on IgG4-related disease.<ii> Curr Opin Rheumatol
</ii>2015;27(1):83-90. [CrossRef] [PubMed]
15 Kashii S. IgG4-Related
disease: a neuro-ophthalmological perspective. <ii>J Neuroophthalmol
</ii>2014;34(4):400-407. [CrossRef] [PubMed]
16 Yu WK, Kao SC, Yang CF, Lee
FL, Tsai CC. Ocular adnexal IgG4-related disease: clinical features, outcome,
and factors associated with response to systemic steroids. <ii>Jpn J
Ophthalmol</ii> 2015;59(1):8-13. [CrossRef] [PubMed]
17 Masaki Y, Shimizu H, Sato
Nakamura T, Nakamura T, Nakajima A, Iwao Kawanami H, Miki M, Sakai T, Kawanami
T, Fujita Y, Tanaka M, Fukushima T. IgG4-related disease: diagnostic methods
and therapeutic strategies in Japan. <ii>J Clin Exp Hematop </ii>
2014;54(2):95-101. [CrossRef]
18 Wong AJ, Planck SR, Choi D,
<ii>et al</ii>. IgG4 Immunostaining and its implications in orbital
inflammatory disease.<ii> PLoS One</ii> 2014;9(10):e109847. [CrossRef] [PubMed] [PMC free article]
19 Kase S, Suzuki Y, Shinohara
T, Kase M. IgG4-related lacrimal sac diverticulitis.<ii> Orbit</ii>
2014;33(3):217-219. [CrossRef]
[PubMed]
20 Khan TT, Halat SK, Al Hariri
AB. Lacrimal gland sparing IgG4-related disease in the orbit. <ii>Ocul
Immunol Inflamm</ii> 2013;21(3):220-224. [CrossRef] [PubMed]
[Top]