·Meta-Analysis· ·Current Issue· ·Achieve· ·Search Articles· ·Online Submission· ·About IJO·
An evaluation of intraoperative and postoperative
outcomes of torsional mode versus longitudinal
ultrasound mode phacoemulsification: a Meta-analysis
Pia Leon1, Ingrid Umari1, Alessandro Mangogna2,
Andrea Zanei1, Daniele Tognetto1
1University Eye Clinic of Trieste, Ospedale
Maggiore, Trieste 34125, Italy
2Department
of Medicine, Surgery and Health Sciences, University of Trieste, Trieste 34149,
Italy
Correspondence to: Pia Leon. University Eye Clinic of Trieste, Ospedale Maggiore, Piazza
dell’Ospitale 1, Trieste 34125, Italy. pialeon@libero.it
Received:
2014-11-12
Accepted: 2015-08-18
Abstract
AIM: To evaluate and compare the intraoperative
parameters and postoperative outcomes of torsional mode and longitudinal mode
of phacoemulsification.
METHODS: Pertinent studies were identified by a computerized
MEDLINE search from January 2002 to September 2013. The Meta-analysis is composed of
two parts. In the first part the intraoperative parameters were considered:
ultrasound time (UST) and cumulative dissipated energy (CDE). The
intraoperative values were also distinctly considered for two categories
(moderate and hard cataract group) depending on the nuclear opacity grade. In
the second part of the study the postoperative outcomes as the best corrected visual acuity (BCVA) and
the endothelial cell loss (ECL) were taken in consideration.
RESULTS: The UST and CDE values
proved statistically significant in support of torsional mode for both moderate
and hard cataract group. The analysis of BCVA did not
present statistically significant difference between the two surgical
modalities. The ECL count was statistically significant in support of torsional
mode (P<0.001).
CONCLUSION: The Meta-analysis shows the superiority of the
torsional mode for intraoperative parameters (UST, CDE) and postoperative ECL
outcomes.
KEYWORDS:
conventional (longitudinal)
phacoemulsification; phacoemulsification; torsional phacoemulsification
DOI:10.18240/ijo.2016.06.18
Citation: Leon P, Umari I, Mangogna A, Zanei A,
Tognetto D. An evaluation of intraoperative and postoperative outcomes of
torsional mode versus longitudinal ultrasound mode phacoemulsification: a
Meta-analysis. Int J Ophthalmol 2016;9(6): 890-897
INTRODUCTION
Phacoemulsification is the gold standard treatment for patients affected
by cataract disease. There has been a recent introduction in significant
technological improvements[1-4].
The latest generation of phacoemulsification machine provides an
efficient and safe treatment due to a variety of options such as the
sophisticated modulation of ultrasonic (US) energy and
improved fluidic control[5-6]. The aim
of cataract surgery is to minimize iatrogenic side effects on ocular structures
as cornea. US energy used during phacoemulsification represents a significant
threat to the endothelial cell integrity especially in patients affected with
hard cataracts[7-12].
In the conventional (longitudinal) mode, the phaco tip moves forward and
backward and the US energy is derived from a longitudinal movement of the tip.
The forward high frequency movement of the tip creates a repulsion effect that
pushes the nucleus away when it moves forward[13-14]. In order to decrease the US energy,
several power modulation modes (pulse, burst, hyperpulse) have been developed[15]. In 2006 torsional US
mode (OZiL, Infiniti Vision System-Alcon Laboratories, Fort Worth, TX, USA) was proposed[16]. This new mode is based on rotary
oscillations of the phacoemulsification tip. The side-to-side movement reduces
the repulsion of the lens fragments minimizing side effects of the procedure[17-19].
In this study we conducted a Meta-analysis of published randomized
controlled trials (RCTs) to evaluate and compare for the first time in
literature the intraoperative parameters and postoperative outcomes of
conventional and torsional phacoemulsification.
MATERIALS AND METHODS
The Meta-analysis was performed accordance with the ethical standards of
the institutional committee on human experimentation and with the Declaration of Helsinki[20-22].
Search Strategy Articles limited to RCTs were identified using a
computerized MEDLINE search from 2002 to September 2013 using the following key
words: “longitudinal phacoemulsification”, “torsional phacoemulsification”,
“longitudinal torsional phacoemulsification” and “conventional torsional
phacoemulsification”.
Inclusion Criteria Two investigators (Leon P, Umari I) independently
viewed the titles and abstracts. Afterwards, the eligible full text articles
were reviewed. Studies that did not meet eligibility criteria in the opinion of
just one of the reviewers were excluded.
Articles were considered for inclusion if they met the following
criteria: RCTs that compared longitudinal and torsional phacoemulsification,
they reported at least one of the intraoperative surgical parameters or
postoperative outcomes measures, only studies performed with human subjects
were included. Language restrictions were imposed; only studies published in
English were considered.
The exclusion criteria were previous significant ophthalmic disease or
complications during surgery or postoperatively. Studies that considered mixed
torsional and longitudinal phacoemulsification modes were excluded.
Data Extraction Two investigators (Leon P, Umari I) independently
selected the studies that fulfilled the inclusion criteria. The following
parameters were taken into consideration: ultrasound time (UST), cumulative
dissipated energy (CDE) for intraoperative parameters and best corrected visual
acuity (BCVA), endothelial cell loss (ECL) for postoperative outcomes.
The UST represents the time in seconds, in which the footpedal remains
in the third position. The mean CDE power indicates the mean percentage of
power spent during the UST. The CDE is calculated in accordance with the
guidelines of the phaco unit manufacturer and by researching previous studies[1,23]. In longitudinal
phaco-mode the CDE was calculated as follows: CDE=mean US power×UST. In torsional mode the CDE was calculated as
follows: torsional amplitude×torsional time×0.4[1].
The coefficient of 0.4 was used because torsional phaco differs from the
conventional mode in two ways: the frequency of the phaco tip in torsional mode
(32 kHz) is 80% of that in the conventional phaco (40 kHz) and the stroke
length of the phaco tip in torsional mode (40 µm) is 50% of that in standard
mode (80 µm)[24].
The UST and CDE values in torsional and phaco modes were automatically
calculated by the device and displayed on the monitor of the phaco system[1].
Intraoperative parameters were extracted from five of seven studies. In
the first analysis, UST and CDE were analyzed separately for all surgeries
performed.
Considering intraoperative parameters (UST, CDE), there was another,
extra analysis performed concerning the nuclear opalescence
(NO) grade. We grouped all the samples on the basis of
nuclear density according to the 3 lens nucleus density grading systems used:
lens opacities classification system II (LOCS II)[25], lens opacities classification system III (LOCS
III)[26] and
the Oxford clinical cataract classification and grading system (OCCCGS)[27]. In particular, in
three[1,16,24] of
the five studies, LOCS II was used, in one[14]
was adopted LOCS III grading and finally Reuschel et al[28] used the OCCCGS. We distinguished a “moderate cataract” group including
≥NOI (Grade-1), ≤NOIII (Grade-3) for LOCSII and ≥NOI (Grade-1), ≤NOIV (Grade-4)
for LOCSIII and “hard cataract” group including ≥NOIV (Grade-4) for LOCSII and
≥NOV (Grade-5) for LOCSIII[14].
In the Reuschel et al[28] study the data of UST
and CDE for each grade of OCCCGS was not provided, so all the samples were
included in both “moderate” and “hard” cataract groups.
Postoperative outcome measures were the mean visual acuity expressed in
the LogMAR scale (BCVA) after 1d and 1mo[1,14,29]
and mean ECL after 1wk, 1 and 3mo[1,14,19,28].
ECL was calculated as ECL=(preoperative cell count-postoperative cell
count)/preoperative cell count×100%[14].
Data from three of the seven studies were taken into consideration to
evaluate the visual acuity after 1d and 1mo. Five studies were included to evaluate the ECL:
three for the analysis of the ECL after 1 and 2wk for the analysis after 1 and 3mo.
The data extracted from each study were title, first author, year of
publication, type of the study, location of trial, number of patients,
patient’s age and sex, outcomes considered, surgical technique,
phacoemulsification machine, grading of nuclear density. Numerical
discrepancies for each of the above were resolved by an independent investigator
(Mangogna
A).
Quality Assessment The quality of each trial was assessed using the Jadad et al[30] scale. The assessment criteria were as follows: 1)
random assignment; 2) appropriateness of randomization; 3) double blind; 4) appropriateness of double blind; 5) clear description and discussion of withdrawals and dropouts. The
total score ranged from 0 to 5. Studies scoring less than 3 points were
considered to be of low quality.
Statistical Analysis The statistical
analysis was performed using “comprehensive meta analysis” software ver. 2.2 (Biostat®, Englewood, NJ, USA). Forest plots
were used to present the results, and the results were expressed as
standardized mean difference (SMD) and 95% confidence interval (CI). The center
of each circle indicated the SMD. The horizontal line bisecting each circle
represented the 95% CI for the SMD. Heterogeneity among studies was tested
using the Chi-squared statistic. If the significant evidence of statistical
heterogeneity or clinical diversity was not found (P>0.10), fixed-effects model was used[31]. However, for the
result showing significant heterogeneity (P<0.10), we used
random-effects model to account for inter-study heterogeneity and tested for
statistically significant difference between the estimates with respect to the torsional and longitudinal modes of
phacoemulsification. Funnel plot was used to
observe the included studies’ publication bias. To explore the steadiness of
our results, sensitivity analysis investigating the influence of each individual
study on the overall Meta-analysis summary estimates was carried out to
identify potential outliners[20,31].
All statistical tests were two-sided.
RESULTS
Literature Search Figure 1 shows the selection process. Overall there were 117 articles
retrieved. Seventy-nine articles were excluded after title and abstract
evaluation. Twenty articles did not fulfill the inclusion criteria. Eleven
trials were duplicate citations so they were excluded. Seven studies published
between 2002 and 2013 were included in this Meta-analysis[1,14,16,19,24,28-29].
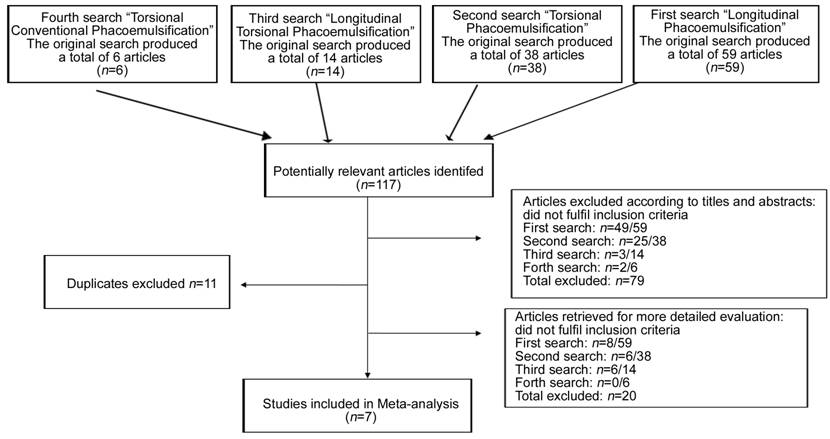
Figure 1 Flow chart of literature search and study
selection.
Characteristics and Quality of Eligible Studies A total of 1765 patients and 1759 eyes (870 treated
with longitudinal phaco-mode, 889 with torsional phaco-mode) were included in
this Meta-analysis. The seven selected studies were performed in seven
different countries: three in Asia (Korea, India, and China), three in Europe
(Germany, Poland and Turkey) and one in Africa (Egypt). Both men and women were
included. Table 1
summarizes characteristics of RCTs included in the
Meta-analysis.
Table 1 Characteristics of included studies in the Meta-analysis
|
Author, year |
Cataract density grading system |
torsionalb |
Intraoperative parameters |
Postoperative outcomes (1wk or 1mo follow-up) |
||||
|
Longitudinal mode |
Torsional mode |
P |
Longitudinal mode |
Torsional mode |
P |
|||
|
Kim et al[14], 2010 |
85 (66.0±9.8) LOCSIII NO≤2, N≤4 NO<4, NO≤5 |
102 51a 51b |
n=34 |
n=33 |
|
n=34 |
n=33 |
|
|
CDE: 5.3±1.65 |
CDE: 2.4±0.64 |
0.014 |
ECL (%): |
ECL (%): |
|
|||
|
UST (s): 61.3±10.0 |
UST (s): 39.1±9.1 |
0.023 |
13.18±11.25 (1wk) |
5.12±4.48 (1wk) |
0.037 |
|||
|
n= 17 |
n=18 |
|
7.92±7.24 (1mo) |
3.19±3.62 (1mo) |
0.128 |
|||
|
CDE: 30.2±5.1 |
CDE: 27.9±9.0 |
0.324 |
n=17 |
n= 18 |
|
|||
|
UST (s): 89.0±13.0 |
UST (s): 48.3±40.1 |
0.249 |
ECL (%): 19.38±16.21 (1wk) |
ECL (%): 24.02±20.24 (1wk) |
0.227 |
|||
|
|
|
|
13.45±16.22 (1wk) |
23.52±22.16 (1wk) |
0.251 |
|||
|
n=51 |
n=51 |
|
||||||
|
BCVA (logMAR): 0.1453 (1mo) |
BCVA (logMAR): 0.2411 (1mo) |
0.273 |
||||||
|
Reuschel et al[28], 2010 |
OCCCGS |
192 94a 98b |
n=94 CDE: 15.18±7.52 UST
(s): 75.13±29.92 |
n=98 CDE: 9.73±6.70 UST
(s): 60.11±31.43 |
<0.001 <0.001 |
n=76 ECL
(%): 7.1±4.4 (3mo) |
n=72 ECL
(%): 7.2±4.6 (3mo) |
0.906 |
|
El-Moatassem et al[16], 2010 |
LOCSII |
200 100a 100b |
n=100 CDE: grade1:
1.35±0.1 grade2:
5.12±1.1 grade3:
10.61±3.2 grade4:
27.571±6.6 UST
(s): grade1:
10.12±3.8 grade2:
23.22±11.3 grade3:
35.14±15.5 grade4:
71.24±11.8 |
n=100 CDE: grade1:
0.65±0.2 grade2:
4.16±2.2 grade3:
9.33±11.8 grade4:
22.02±9.7 UST (s): grade1: 3.25±0.4 grade2: 20.43±5.3 grade3: 28.41±12.7 grade4: 53.19±27.3 |
<0.01 >0,05 >0.05 <0.05 <0.01 >0.05 >0.05 <0.01 |
N.A. |
N.A. |
- |
|
Rekas et al[29], 2009 |
LOCSII |
400 196a 204b |
n=196 CDE: grade1: 5.16±0.17 grade2: 6.43±0.12 grade3: 7.67±0.27 grade4: 7.92±0.28 |
n=204 CDE: grade1:
1.58±0.13 grade2:
3.01±0.14 grade3:
5.83±0.28 grade4:
7.11±0.63 |
<0.000001 <0.000001 0.000002 0.246796 |
BCVA (logMAR): 0.21±0.09
(1wk) 0.07±0.06
(1mo) |
BCVA (logMAR): 0.19±0.10
(1wk) 0.06±0.05
(1mo) |
>0.05 >0.05 |
|
Vasavada et al[19], 2010 |
Emery’s
Classification 1-5 (cLegacy
Everest, Alcon Laboratories) |
360 120a (120c) 120b |
n=120 surgical time (min): 6.65±2.48 n=120c surgical time (min): 7.05±3.38 |
n=120 surgical time (min): 4.40±1.37 n=120 surgical time (min): 4.40±1.37 |
<0.05 <0.05 |
n=120 ECL (%) 5.6±2.5 (3mo) n=120c 5.8±2.6 (3mo) |
n=120 ECL (%) 3.3±0.8 (3mo) n=120 3.3±0.8 (3mo) |
<0.001 <0.001 |
|
Bozkurt et al[24], 2009 |
LOCSII |
100 47a 53b |
n=47 CDE:
29.9±16.9 USTT
(min): 1.62±1.06 |
n=53 CDE:
25.2±19.1 USTT
(min): 1.49±0.98 |
0.20 0.55 |
ECL
(%) 6.7±3.3
(1wk) |
ECL
(%) 4.2±5.7
(1wk) |
0.56 |
|
Liu et al[1], 2007 |
LOCSII |
525 262a 263b |
n=262 CDE: grade1:
1.25±0.5 grade2:
4.18±1.2 grade3:
8.59±6.5 grade4:
16.51±9.6 UST
(s): grade1:
10.25±7.4 grade2:
25.14±5.5 grade3:
36.45±8.3 grade4:
61.44±17.8 |
n=263 CDE: grade1:
0.94±0.3 grade2:
3.13±2.7 grade3:
7.47±12.6 grade4:
14.08±8.3 UST (s): grade1: 8.32±6.8 grade2: 18.45±7.2 grade3: 29.48±12.4 grade4: 48.39±20.3 |
<0.05 <0.05 <0.05 <0.05 <0.05 <0.05 <0.05 <0.05 |
BCVA (logMAR) 0.00±0.10 (1wk) -0.10±0.07 (1mo) ECL (%) 435±472 (1wk) 567±513 (1mo) |
BCVA (logMAR) -0.08±0.05 (1wk) -0.12±0.06 (1mo) ECL (%) 320±378 (1wk) 467±523 (1mo) |
<0.001 >0.01 <0.05 <0.05 |
Intraoperative parameters (UST, CDE) were examined in five of the seven
studies. Postoperative outcomes were evaluated as follows: BCVA was evaluated
after 1, 30d in three of the seven studies, and ECL was evaluated after 1wk, 1
and 3mo in five of the seven studies.
Intraoperative Results Five of the seven studies were included in the evaluation of
intraoperative parameters for a total of 1119 eyes.
Ultrasound Time Five studies reported UST[1,14,16,24,28]. Examination of the forest plot showed that the mean
UST was shorter in the torsional group than in the longitudinal group. Analysis
of these data showed that the SMD in UST (Figure 2) was statistically significant (SMD=-0.708; 95% CI, -0.833
to -0.584, P=0.00).

Figure 2 Forest plot comparison of mean UST Subgroup based on nuclear opacity grade (NO).
Cumulative Dissipated Energy Five studies reported the data for mean CDE during cataract
surgery[1,14,16,24,28].
Examination of the forest plot showed that the mean CDE was lower in the
torsional group in all studies considered. Analysis of these data showed that
the SMD in CDE (Figure 3) was statistically significant (SMD=-0.533; 95% CI, -0.656
to -0.409, P=0.00).
Figure 3 Forest plot comparison of mean CDE Subgroup based on nuclear
opacity
(NO) grade.
Ultrasound Time and Cumulated Dissipated Energy for Moderate and Hard Cataract Groups Patients were also divided into two groups according
to the lens nucleus density grade: moderate and hard cataract. A total of 1119 eyes, five of seven studies[1,14,16,24,28],
were divided as follow: the moderate cataract group was composed of 925 eyes
and the hard cataract group was made up of 194 eyes.
The UST and CDE values were found to be statistically significant in
support of the torsional mode for both moderate and hard cataract group. The SMD
for moderate cataracts were of -0.697 (95% CI, -0.834 to -0.560; P=0.000) and -0.586 (95% CI, -0.724 to -0.449, P=0.000) for UST and CDE respectively (Figure 4). Advanced
cataract presented a SMD of -0.623 (95% CI, -0.828 to -0.417, P=0.000) for UST and of -0.527 (95% CI, -0.731 to -0.323, P=0.000) for CDE (Figure 5).

Figure 4 Forest plot comparison of mean UST and mean
CDE for moderate cataract group A: Forest plot comparison of mean UST for moderate cataract group; B: Forest plot comparison of mean CDE for moderate cataract group. Subgroup
based on nuclear opacity (NO)
grade.

Figure 5 Forest plot comparison of mean UST and mean
CDE for hard cataract group A: Forest plot comparison of mean UST for hard cataract group; B: Forest plot comparison of mean CDE for hard cataract group.
Postoperative Outcomes Visual Acuity Three studies for a total of 1027 eyes
reported BCVA (logMAR expressed) at 1
and 30d postoperatively[1,14,29].
Analysis of these data revealed that the SMD in BCVA were not statistically
significant at 1d (P=0.87) and 1mo (P=0.69).
Endothelial Cell Loss Five studies for a total of 1279 eyes were used for the evaluation of
the ECL after surgery[1,14,19,24,28]. Three studies were included for analysis at 1wk, two
for analysis at 1, 3mo (Figure 6). The mean preoperative endothelial
cell count (ECC) reported was not statistically different among the studies.
The analysis with results in all cases (1wk, 1 and 3mo of follow-up) showed
that the SMD were statistically different in favour of torsional mode (P<0.01).
Figure 6 Forest plot
comparison of ECL A: After 1wk; B: 1mo; C: 3mo.
Heterogeneity The test of heterogeneity is used to determine whether
there are genuine differences underlying the results of the studies
(heterogeneity) or whether the variation in findings is compatible with chance
alone (homogeneity).
In the present Meta-analysis, a statistical heterogeneity was detected in some outcome measures (P<0.10). Heterogeneity may be
explained by the variability in the participants (i.e. patient characteristics, sample size) or interventions (i.e. make and model of the
phacoemulsification machine, surgical skills).
Publication Bias The funnel plot showed no correlation between study
size and effect.
DISCUSSION
Reviewing the data from seven RCTs this Meta-analysis provides evidence that there was a significant difference between torsional and
longitudinal phacoemulsification in intraoperative parameters for all five of
the studies considered and secondary for both moderate and hard cataract
subgroups. To our knowledge there are no other Meta-analysis studies published
that compare these two phaco techniques. From our analysis, UST was shorter and
CDE was lower in torsional modality. There was also significant difference in
ECL in favour of torsional mode. There were no reported significant
intraoperative or postoperative complications in any studies. BCVA was not
statistically significant between the two groups.
We systematically compared the efficiency of the techniques by analysing
the UST and the CDE. Increasing the effectiveness of phacoemulsification
reduces the total ultrasound power delivered to the anterior segment, which
leads to less surgical tissue damage and less corneal edema[32-33]. US power is considered a risk factor for ECL[7], and the use of high US energy is associated with
heat generation damage to the endothelium[8].
This Meta-analysis showed that the mean UST was statistically
significantly shorter (P=0.00) and
the mean CDE was statistically significantly lower (P=0.00) in the torsional group than in the longitudinal group. In this Meta-analysis we also compared the efficacy of
torsional mode with longitudinal phacoemulsification in different grades of
nucleus densities. The UST and CDE values
proved statistically significant in support of the torsional mode for both the
moderate and hard cataract groups (P=0.00
in all groups). Our results demonstrate that
torsional phacoemulsification produces an efficient mode of phacoemulsification
with reduced mean UST and CDE in all grades of nucleus densities especially in
hard cataracts (Grade 4 for LOCSII and Grade 5 for LOCS III). Our results are
supported by those findings obtained by all studies included. This was
reflected in the absence or traces of corneal edema but this parameter was not
analyzed because the data were not provided in all studies and the corneal ECC was more preserved in the torsional group. In fact, comparing the two phacoemulsification modalities,
longitudinal demonstrated a higher value of intraoperative parameters and a
greater level of ECL.
Several preoperative and intraoperative parameters (nucleus grade, UST,
CDE) can affect ECL after phacoemulsification[7,34]. There was a significant difference in ECL
postoperatively after 1wk, 1 and 3mo (P<0.01).
The mean preoperative ECC reported was not statistically different among the
studies (P<0.01).
Good, fast, and stable visual rehabilitation is the goal of cataract
surgery, and BCVA is one of the best parameters to evaluate the quality and
efficiency of a surgical technique[35].
Our Meta-analysis showed no statistically differences in BCVA at 1d and
1mo in torsional and longitudinal group and both had better BCVA
postoperatively. Liu et al[1] report that although the
BCVA at 1d and 7d was significantly better in the torsional group, this
advantage did not remain at 30d. This suggests that the torsional mode has a
better visual outcome in the early postoperative phase. This pattern of visual
rehabilitation after surgery is probably attributable to the corneal injury and
its recovery[1].
Complications which occurred during cataract surgery such as capsular
tears, leaking corneal incision, posterior capsular rupture were not considered
in our Meta-analysis due to a lack of data. The limitations of this Meta-analysis
stem from the design of the individual trials and the methods of a
Meta-analysis. First, a limitation of this
Meta-analysis is that only published studies searched on Medline were included.
Although multiple databases and websites were explored, unfortunately, it is
possible that we may have failed to include some papers, especially those
published in other languages. A specific limitation of this analysis is that
many trials lacked adequate allocation concealment, blinding, different nuclear
opacity grading systems and sample size assessment, which may leave them
vulnerable to bias and misestimation of the beneficial effects of one surgical
technique. Finally, the pooled data of longitudinal and torsional
phacoemulsification modalities are based on only seven papers. Therefore, more
research is still needed on the available guidance derived from the current
literature.
Our Meta-analysis and other clinical evidences suggests
that the torsional and longitudinal phacoemulsification are both safe methods of
removing uncomplicated senile cataract but torsional mode is an improved
ultrasound phacoemulsification modality with increased efficacy and safety that
provides intraoperative time savings and good postoperative outcomes in regard
to ECL and corneal condition when compared to the traditional modulated
longitudinal ultrasound.
ACKNOWLEDGEMENTS
The
paper has been
presented at the “XV Congress of the AICCER-Italian Association of Cataract
& Refractive Surgeons” (15-17 March 2012, Trieste, Italy); the “XXX Congress
of the ESCRS-European Society of Cataract & Refractive Surgeons” (8-12
September 2012, Milan, Italy); the “18th ESCRS Winter
Meeting-European Society of Cataract & Refractive Surgeon” (14-16 February
2014, Ljubljana, Slovenia).
Conflicts of Interest: Leon P, None; Umari
I, None; Mangogna A, None; Zanei A, None; Tognetto D, None.
REFERENCES
1 Liu Y, Zeng M, Liu X, Luo L, Yuan Z, Xia Y, Zeng
Y. Torsional mode versus conventional ultrasound mode phacoemulsification;
randomized comparative clinical study. J
Cataract Refract Surg 2007;33(2):287-292. [CrossRef]
[PubMed]
2 Hoffman RS, Fine IH, Packer M. New
phacoemulsification technology. Curr Opin
Ophthalmol 2005;16(1):38-43. [CrossRef]
3 Mackool RJ, Brint SF. AquaLase: a new technology
for cataract extraction. Curr Opin
Ophthalmol 2004;15(1):40-43. [CrossRef] [PubMed]
4 Gimbel HV, da Reitz Pereira C. Advances in
phacoemulsification equipment. Curr Opin
Ophthalmol 2002;13(1):30-32. [CrossRef] [PubMed]
5 Fishkind W, Bakewell B, Donnenfeld ED, Rose AD,
Watkins LA, Olson RJ. Comparative clinical trial of ultrasound
phacoemulsification with and without the WhiteStar system. J Cataract Refract Surg 2006;32(1):45-49. [CrossRef]
[PubMed]
6 Praveen MR, Vasavada AR, Shah R, Vasavada VA.
Effect of room temperature and cooled intraocular irrigating solution on the
cornea and anterior segment inflammation after phacoemulsification: a
randomized clinical trial. Eye
2009;23(5):1158-1163. [CrossRef] [PubMed]
7 O’Brien PD, Fitzpatrick P, Kilmartin DJ, Beatty
S. Risk factor for endothelial cell loss after phacoemulsification surgery by a
junior resident. J Cataract Refract Surg
2004;30(4):839-843. [CrossRef]
8 Sippel KC, Pineda R Jr. Phacoemulsification and
thermal wound injury. Semin Ophthalmol 2002;17(3-4):102-109. [CrossRef]
[PubMed]
9 Ernest P, Rhem M, McDermott M, Lavery K, Sensoli
A. Phacoemulsification conditions resulting in thermal wound injury. J Caract Refract Surg
2001;27(11):1829-1839. [CrossRef]
10 Chen X, Ji Y, Lu Y. Comparison of clear corneal
incision injuries between torsional and conventional phacoemulsification. Graefes Arch Clin Exp Ophthalmol 2013;251(9):2147-2154. [CrossRef]
[PubMed]
11 Kaushik S, Ram J, Brar GS, Bandyopadhyay S.
Comparison of the thermal effect on clear corneal incision during phacoemulsification
with different generation machines. Ophthalmic
Surg Lasers Imaging 2004;35(5):364-370. [PubMed]
12 Bradley MJ, Olson RJ. A survey about
phacoemulsification incision thermal contraction incidence and causal
relationships. Am J Ophthalmol
2006;141(1):222-224. [CrossRef] [PubMed]
13 Zacharias J. Role of cavitation in the
phacoemulsification process. J Cataract
Refract Surg 2008;34(5):846-852. [CrossRef]
[PubMed]
14 Kim DH, Wee WR, Lee JH, Kim MK. The comparison
between torsional and conventional mode phacoemulsification in moderate and
hard cataracts. Korean J Ophthalmol 2010;24(6):336-340. [CrossRef]
[PubMed]
[PMC free article]
15 Baykara M, Ercan I, Ozçetin H. Microincisional
cataract surgery (MICS) with pulse and burst modes. Eur J Ophthalmol 2006;16(6):804-808. [PubMed]
16 El-Moatassem Kotb AM, Gamil MM. Torsional mode
phacoemulsification: effective, safe cataract surgery technique of the future. Middle East Afr J Ophthalmol 2010;17(1):69-73. [PMC free article] [PubMed]
17 Solomon K. Performance
of the Infiniti system: torsional vs conventional phacoemulsification handpieces.
Paper presented at: annual meeting of the american society of cataract and
refractive surgery. March 17-22, 2006;San Francisco, CA, USA.
18 Boukhny M. Laboratory
performance comparison of torsional and conventional longitudinal phacoemulsification.
Paper presented at: annual meeting of the american society of cataract and
refractive surgery. March 17-22, 2006;San Francisco, CA, USA.
19 Vasavada AR, Raj SM, Patel U, Vasavada V,
Vasavada V. Comparison of torsional and microburst longitudinal
phacoemulsification: a prospective randomized, masse clinical trial. Ophthalmic Surg Lasers Imaging 2010;41(1):109-114.
[CrossRef] [PubMed]
20 Egger M, Smith GD, Phillips AN. Meta-analysis:
principles and procedures. BMJ
1997;315(7121):1533-1537. [CrossRef]
21 Pogue J, Yusuf S. Overcoming the limitations of
current meta-analysis of randomized controlled trials. Lancet 1998;351(9095):47-52. [CrossRef]
22 Sacks HS, Berrier J, Reitman D, Ancona-Berk VA,
Chalmers TC. Meta-analyses of randomized controlled trials. N Engl J Med 1987;316(8):450-455. [CrossRef]
[PubMed]
23 Zeng M, Liu X, Liu Y, Xia Y, Luo L, Yuan, Z,
Zeng Y, Liu Y. Torsional ultrasound modality for hard nucleus
phacoemulsification cataract extraction. Br
J Ophthalmol 2008;92(8):1092-1096. [CrossRef] [PubMed] [PMC free article]
24 Bozkurt E, Bayraktar S, Yazgan S, Cakir M, Cekic
O, Erdogan H, Yilmaz OF. Comparison of conventional and torsional mode (OZil)
phacoemulsification: randomized prospective clinical study. Eur J Ophthalmol 2009;19(6):984-989. [PubMed]
25 Chylack LT Jr, Leske MC, McCarthy D, Khu P,
Kashiwagi T, Sperduto R. Lens opacities classification system II (LOCS II). Arch Ophtalmol 1989;107(7):991-997. [CrossRef]
26 Chylack LT Jr, Wolfe JK, Singer DM, Leske MC,
Bullimore MA, Bailey IL, Friend J, McCarthy D, Wu SY. The Lens Opacities
Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol 1993;111(6):831-836. [CrossRef] [PubMed]
27 Hall AB, Thompson JR, Deane JS, Rosenthal AR.
LOCS III versus The Oxford Clinical Cataract Classification and Grading Sysytem
for the assessment of nuclear, cortical and posterior subcapsular cataract. Ophthalm Epidemiol 1997;4(4):179-194. [CrossRef]
28 Reuschel A, Bogatsch H, Barth T, Wiedemann R.
Comparison of endothelial changes and power settings between torsional and
longitudinal phacoemulsification. J
Cataract Refract Surg 2010;36(11):1855-1861. [CrossRef]
[PubMed]
29 Rekas M, Montés-Micó R, Krix-Jachym K, Kluś A,
Stankiewicz A, Ferrer-Blasco T. Comparison of torsional and longitudinal modes
using phacoemulsification parameters. J
Cataract Refract Surg 2009;35(10):1719-1724. [CrossRef]
[PubMed]
30 Jadad AR, Moore RA, Carroll D, Jenkinson C,
Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of
randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17(1):1-12. [CrossRef]
31 Thomas J, Graziosi S, Hiqqins S, Coe R,
Torgerson C, Newman M. Teaching meta-analysis using MetaLight. BMC Res Notes 2012;5:571. [CrossRef] [PubMed] [PMC free article]
32 Alió J, Rodríguez-Prats JL, Galal A, Ramzy M.
Outcomes of microincisional cataract surgery versus coaxial
phacoemulsification. Ophthalmology
2005;112(11):1997-2003. [CrossRef]
[PubMed]
33 Takahashi H. Free radical development in
phacoemulsification cataract surgery. J
Nippon Med Sch 2005;72(1):4-12. [CrossRef]
34 Ataş M, Demircan S,
Karatepe Haşhaş AS, Gülhan A, Zararsız G. Comparison of corneal endothelial
changes following phacoemulsification with transversal and torsional
phacoemulsification machines. Int J
Ophthalmol 2014;7(5):822-827.
35 Can I, Takmaz T, Yildiz Y, Bayhan HA, Soyugelen
G, Bostanci B. Coaxial, microcoaxial, and biaxial microincisional cataract
surgery: prospective comparative study. J
Cataract Refract Surg 2010;36(5):740-746. [CrossRef]
[PubMed]
[Top]