INTRODUCTION
Thanks to continuous improvements in technology and surgical techniques cataract surgery has become a safer and more efficient procedure over the years. An important role in the evolution of this surgery has been the chance to perform the entire procedure through smaller clear corneal incisions(CCI), thus allowing safer surgery and faster visual recovery for the patients resulting in better outcomes[1]. Nowadays technological innovations and the bimanual microincision cataract surgery (B-MICS) technique permits the surgical procedure through CCIs which are smaller than 2.0 mm[2].
B-MICS is a micro-invasive variant of the traditional coaxial phacoemulsification (C-MICS) and it is characterized by the separation of the aspiration and the infusion probes which permits microincisions of 1.4 mm[3-4]. For this reason we believe that this is an ideal technique for cataract extraction due to increased anterior chamber stability, lower postoperative inflammation, reduced surgically induced astigmatism (SIA)and rapid incision healing[1,3-7].
The implantation of the intraocular lens (IOL) is usually performed with an enlargement of the main CCI from 1.4 to 1.8 or 2.2 mm; this leads to the instability of the corneal incision because in the B-MICS technique it is a monoplanar incision. The innovative aspheric Incise® MJ14 IOL (Bausch& Lomb, Rochester, NY, USA) can be implanted through a 1.4 mm CCI using a wound-assisted technique which allows surgeons to perform the entire procedure without an enlargement of the main incision. This characteristic has brought to the forefront the B-MICS technique. This procedure may offer further advantages to the surgeon, such as minor inflammation and major micro incision stability. Moreover, the Incise IOL, thanks to its higher hydrophobic polymer content,could cause less posterior capsule opacification (PCO) then other IOLs created for micro incisions.
The aims of our study were to evaluate visual outcomes, PCO incidence and morphological features of 1.4 mm CCIs in eyes implanted with the Incise® MJ14 IOL, comparing the results with those obtained with the Akreos® MI60 IOL implantation through an enlarged 1.8 mm CCI; all patients underwent cataract surgery using the B-MICS technique with an 18mo follow-up.
SUBJECTS AND METHODS
In this prospective comparative study, we evaluated 80 eyes of 80 patients who underwent cataract extraction at the Institute of Ophthalmology, University of Modena &Reggio Emilia. Group A was represented by 40 consecutive cases carried out using the B-MICS technique and Incise®IOL MJ14 implantation though a 1.4 mm CCI; group B was represented by 40 consecutive cases carried out using the B-MICS technique and Akreos® MI60 implantation though a 1.8 mm enlarged CCI. Patients in both groups were similar for preoperative parameters, age and cataract characteristics.The study adhered to the tenets of the Declaration of Helsinki and was approved by the local Ethics Committee. All patients provided informed consent in written form before surgery and did not receive a stipend. Inclusion criteria was the presence of cataract from grade 2 to 3 on the Lens Opacities Classification System III (LOCSIII). Exclusion criteria were previous surgery, complicated cataract (e.g. total cataract,traumatic cataract), concomitant pathology (uveitis, glaucoma,corneal opacities), insufficient mydriasis (<4.0 mm), and a low endothelial cell count (<1500 cells/mm2). Patients with one eye only were also excluded.
Prior to surgery all patients underwent a careful clinical history evaluation, best corrected visual acuity (BCVA) examination,anterior segment biomicroscopy, fundus evaluation, biometry(IOLMaster, Carl Zeiss Meditec AG, and US500 Echoscan, Nidek Technologies Srl), corneal biomicroscopy (Noncon Robo, Konan Medical), and corneal topography (CT1000, Shin-Nippon).
Prophylactic strategies to prevent infections included application of topical antibiotic eyedrops before surgery,application of povidone-iodine 5.0 to the conjunctival cul-de-sac,preparation of the periocular skin with povidone-iodine 10.0,careful sterile draping of the eyelid margins and eyelashes,instillation of intracameral antibiotics at the end of surgery and application of topical antibiotic eyedrops after surgery.
All patients underwent uneventful phacoemulsification cataract surgery with implantation of a posterior chamber IOL performed by the same surgeon (Cavallini GM) using the B-MICS technique. Mydriasis was obtained by instilling phenylephrine 10.0. Topical anesthesia was achieved using benoxinate hydrochloride eyedrops (solution 4 mg/mL). In all cases,a balanced salt solution for irrigation and sodium hyaluronate 1.2% (Amvisc) were used. Two 1.4 mm trapezoidal incisions were created in clear cornea at 10 o'clock and 2 o’clock with a pre-calibrated refined diamond knife (1.3 to 1.2 mm). A continuous curvilinear capsulorhexis (CCC) with a diameter of between 5.0 and 6.0 mm was made with a capsulorrhexis forceps (E. Janach srl instruments). Hydro-dissection was performed with a 26-gauge cannula and phacoemulsification with a 20-gauge 30-degree angled sleeveless probe and an irrigating chopper (E. Janach srl instruments). Phaco-fracture was obtained using the stop- and chop technique, with the surgeon holding the phaco probe in the dominant hand.Irrigation/aspiration (I/A) was performed with a 21-gauge probe with an oval-shaped section (Bausch & Lomb, Inc.)introduced through the microincisions. The surgeon always carried out an accurate cleaning of the posterior capsule at the end of I/A with a manual aspiration cannula or bimanual I/A.In group A an Incise® MJ14 IOL was directly implanted through the original 1.4 mm wide incision with a woundassisted technique without main incision enlargement. The injection system was the new ViscoJectTM BIO 1.5 mm(inner diameter 0.9 mm, outer diameter 1.3 mm, Medicel AG).Incise® MJ14 is an aspheric, acrylic, hydrophilic IOL with 22%water content, 360° barrier edge with a radius of curvature of 5 microns and a 4-point-fixation-haptic design. Thanks to the higher hydrophobic polymer content, this IOL has a plastic behavior that causes a slow opening in the bag. It is designed to be implanted through a 1.8 mm CCI in the bag or a 1.4 mm CCI wound-assisted technique. The overall diameter is 11.00 mm and the optic body diameter is 6.0 mm at 20.0 D. In group B the main incision was enlarged to 1.8 mm with a precalibrated knife (Alio MICS multi-incision knife, Katena Inc.)and an Akreos® MI60 IOL was implanted using the woundassisted technique. The injection system was the ViscoJectTM BIO 1.8 mm (Medicel AG). Akreos® MI60 is an aspheric,acrylic, hydrophilic IOL with 26% water content, square edge design, 10° angulation and a 4-point-fixation-haptic design.It is designed to be implanted through a 1.8 mm CCI woundassisted technique and does not have any hydrophobil polymer content. The overall diameter is 10.5-11.0 mm and the optic body diameter is 6.0 mm at 20.0 D. At the end of surgery the ocular viscoelastic device (OVD) was removed and the incisions were hydrated for safety reasons. Postoperative therapy consisted of tobramycin and dexamethasone eye-drops 4 times a day for 15d followed by flurbiprofen eyedrops 3 times a day for a further 15d (Figure 1).
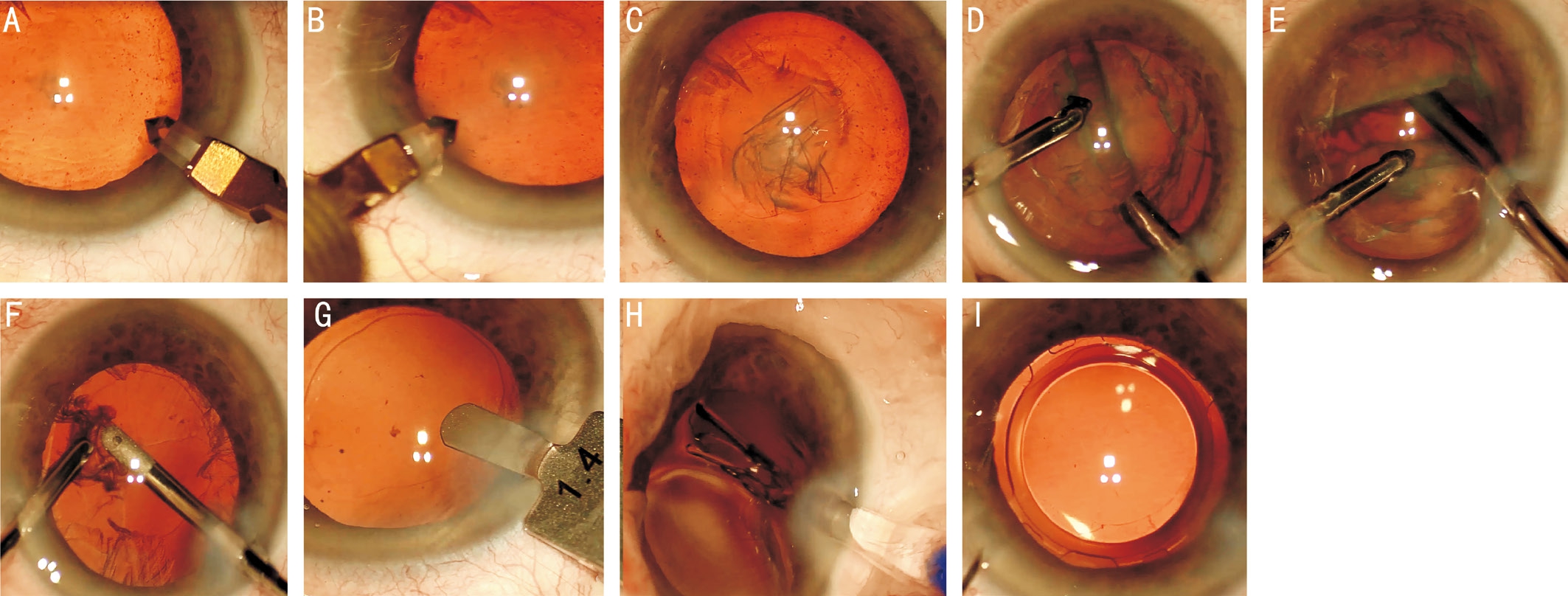
Figure 1 B-MICS technique A: Main microincision; B: Secondary microincision: C: Capsulorhexis; D, E: Micro phacoemulsification; F:Irrigation/aspiration; G: Measurement of the main CCI width; H: IOL implantation; I: IOL in the bag.
In the postoperative follow-up, all patients underwent BCVA evaluation, endothelial biomicroscopy, corneal topography,anterior segment-optical coherence tomography (AS-OCT),slit-lamp examination with anterior segment photograph and fundus evaluation. All clinical parameters have been reported and analyzed. These follow-up assessments were performed at 7, 30d, 6 and 18mo after surgery. All the examinations were performed by the same experienced physician.
PCO was evaluated with the computer-based software evaluation of posterior capsule opacification 2000 (EPCO2000, Incl.Merge, Creative Development, CA, USA) introduced in 1997 by Tetz et al[8]. This software is based on morphological assessment of PCO and allows a quantitative and qualitative evaluation of the amount of IOL surface affected by opacification. For every patient we took retro-illumination images of the pseudophakic anterior segments of the eyes affected, after dilation of the pupil. We used a camera connected to the slit-lamp, and then we used EPCO2000 to evaluate each picture which gave us a final PCO-score for every eye examined. The PCO score for each eye is calculated by multiplying the density of the opacification, graded from 0 (none) to 4 (severe) by the fractional PCO area involved behind the entire IOL optics. Density areas were identified and marked interactively by the observer on the computer screen.The evaluation was always carried out by the same expert observer. PCO scores of the two groups were compared during the follow-up schedule.
For CCI evaluation, AS-OCT examination (OptosOCT SLOTM) was performed by the same examiner at 1, 3, 7, 30d and 6, 18mo postoperatively on both the main and the secondary incision. Five raster lines from every incision were selected and analyzed by 2 independent operators. The examiners looked for evidence of the five morphological features previously described in several recent studies: epithelial gaping of the wound, endothelial gaping of the wound, misalignment of the roof and floor of the incision on the endothelial side,Descemet membrane detachment and loss of coaptation along the stromal tunnel[9-12]. We compared 1.4-mm incision results with Incise® IOL implantation versus 1.8-mm enlarged incision results with Akreos® MI60 IOL implantation. Both temporal and nasal incisions were analyzed using AS-OCT; all images were then exported, examined and measured.
All data have been recorded in an Excel database (Microsoft Excel 2010, Microsoft Office Professional Plus 2010) and for analysis we used Stata 13.1 software (StataCorp, College Station, TX, USA) with Student’s t test and WilCoxon ranksum test. P<0.05 was taken to indicate statistical significance.
RESULTS
For group A 40 eyes (19 right eyes and 21 left eyes) of 40 patients (18 males and 22 females) were included in the study; the average age was 74±9.0y (range 54-90y). An Incise® MJ14 IOL was implanted in every eye. All IOLs were implanted in the bag. We recorded a mean total surgical time of 17.76±4.98min. Mean final size of the incision was 1.42±0.08 mm. For group B 40 eyes (21 right eyes and 19 left eyes) of 40 patients (19 males and 21 females) were included in the study; the average age was 74±7.0y (range 54-90y). An Akreos MI60 IOL was implanted in every eye in the bag. We recorded a mean total surgical time of 16.21±5.07min. Mean final size of the enlarged incision was 1.74±0.11 mm. Table 1 shows the demographic data and pre- and post-operative results.
There was no statistically significant difference between the preoperative BCVA of group A and group B (P=0.28).In group A, we found a statistically significant mean BCVA improvement from baseline to 18mo (0.509±0.249 logMAR).In the control group (group B), we found a statistically significant mean BCVA improvement from baseline to 18mo of 0.410±0.332 logMAR. The improvement of visual acuity during the follow-up showed a not-statistically significant difference between the two groups (P=0.22).
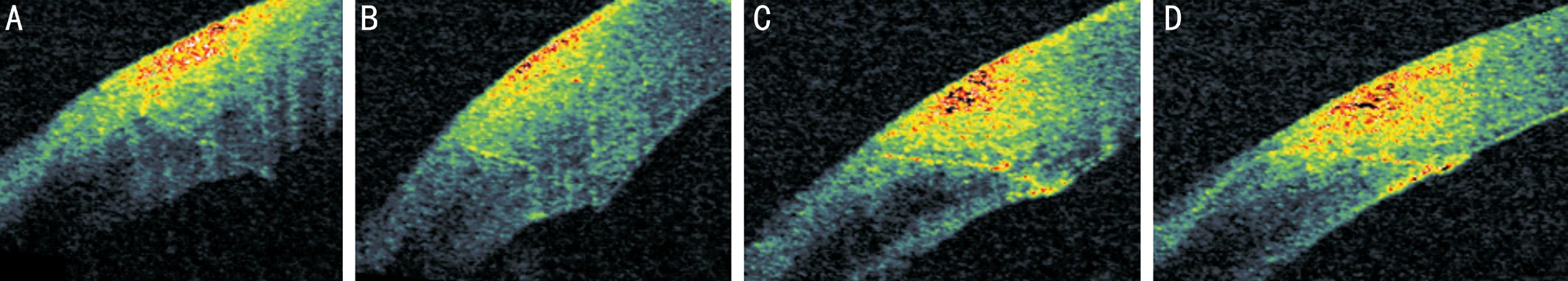
Figure 2 Morphology of a 1.4 mm CCI at 1 (A), 3 (B), 7 (C), 30d (D) after surgery.
Table 1 Demographic data and mean results at baseline and during the follow-up at 30d, 6 and 18mo
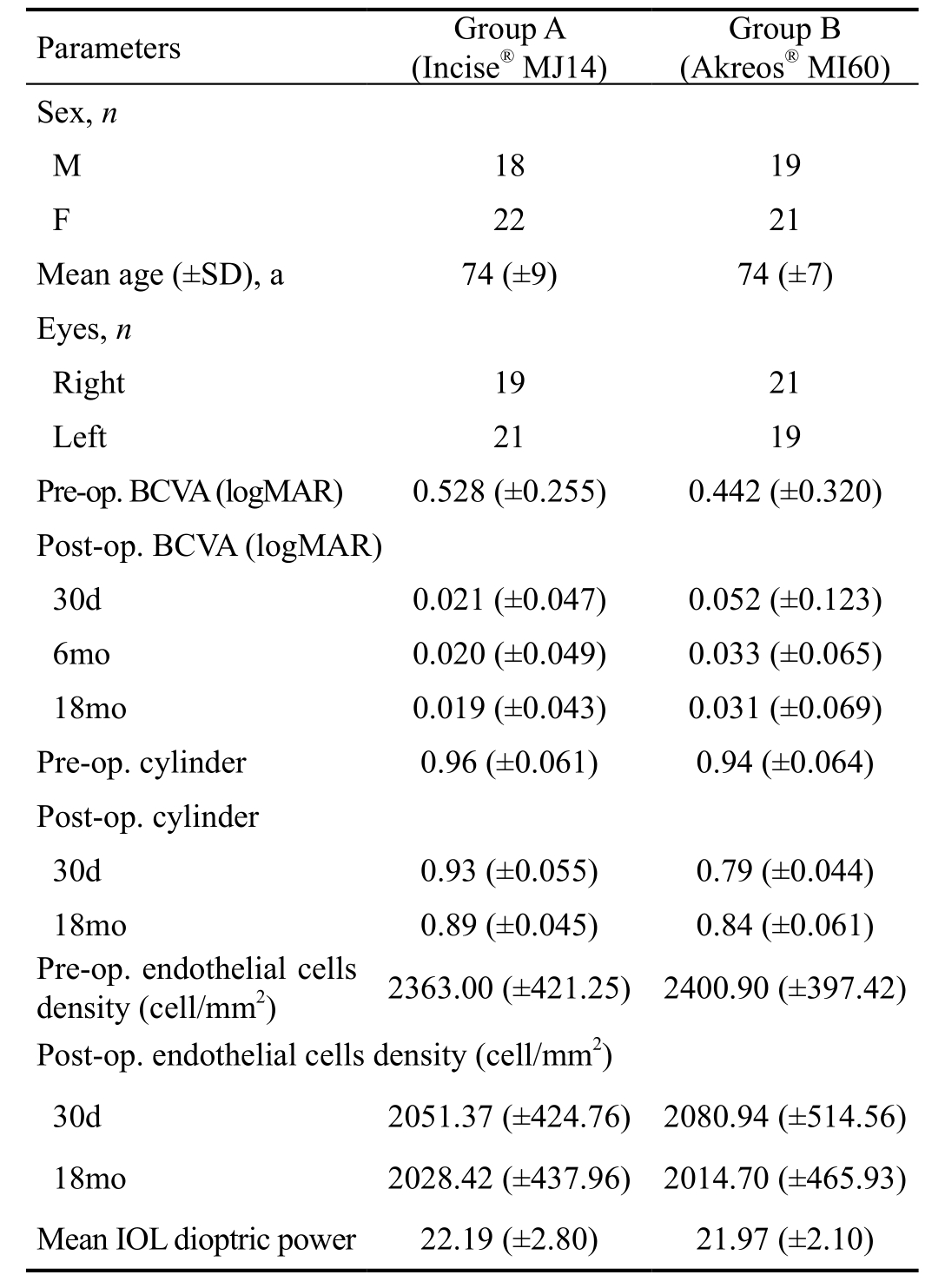
With regard to SIA, in group A we found a mean decrease of 0.07±0.43 diopters at 18mo after surgery while for group B this was 0.09±0.51, both not statistically significant.The comparison between the two groups did not show any significant difference (P=0.49). Preoperative mean endothelial cell density was 2363.00±421.25 cell/mm2 in group A and 2400.90±397.42 cell/mm2 in group B; postoperatively mean endothelial cell count at 30d was 2051.37±424.76 cell/mm2 in group A and 2080.94±514.56 cell/mm2 in group B and at 18mo it was 2028.42±437.96 cell/mm2 in group A and 2014.70±465.93 cell/mm2 in group B. Group A presented a mean cell loss of 334.58±466.42 cell/mm2 (14.16%), whereas group B presented a mean cell loss of 386.20±340.47 cell/mm2(16.08%) at 18mo; in both cases the results were statistically significant (P<0.05) with no significative difference between the two groups (P=0.69). No severe complications were reported during the follow-up in both groups at slit-lamp evaluation. The day after surgery 9 patients in group A (22.5%)and 4 patients in group B (10.0%) presented a slight corneal edema near the main CCI site (P=0.13). These alterations completely disappeared in the first week of follow-up in both groups. At AS-OCT the most common architectural alterations were endothelial gaping and local detachment of Descemet’s membrane; these showed a progressive reduction during the follow-up (Table 2; Figure 2).
As regards main incision analysis, we found a statistically significant difference in the first days of follow-up between the two groups with greater incidence of endothelial gap (P=0.03)and local detachment of Descemet’s membrane (P=0.02) in group B. These alterations were present more significantly in the main incision rather than in the secondary incision for each group.
Regarding PCO evaluation, in group A we did not record any sign of IOL opacification before 30d of follow-up. The first signs of epithelial lens cells proliferation were detected at 6mo and this was not associated with any reduction in BCVA. The PCO score at the 18-month follow-up was higher in group B(0.08±0.18) than in group A (0.03±0.07) but the difference was not statistically significant (P=0.11). We did not find any clinically significant PCO with consequent significant visual acuity reduction at 18mo; despite a few cases with a mild involvement of the visual axis, Nd:YAG laser capsulotomy was not necessary in any case of the two groups during the follow-up.
DISCUSSION
This study investigated the post-operative results, the PCO incidence and the CCI architecture obtained by an expert surgeon using B-MICS with the new aspheric MJ14 Incise®IOL implanted through a 1.4 mm CCI without enlarging the main incision; we compared the results with those obtained by the same expert surgeon with the Akreos® MI60 implanted through a 1.8-mm enlarged main incision.
With regard to postoperative results, we found a significant increase in BCVA during the follow-up as has been previously reported in literature[13], without significant difference between the two groups. We did not find any difference in SIA between the two groups. Our findings on endothelial cell loss were statistically significant with a reduction of cells in the postoperative follow-up which was similar for the two groups(Table 1).
Table 2 CCIs morphological features along the follow-up %

M: Main incision; S: Secondary incision.
AS-OCT allows a non-invasive in vivo analysis of CCIs[14-17].Several recent studies on the architecture of CCIs are focused on the five morphological features first described in 2007 by Calladine and Packard[9]: epithelial gaping of the wound,endothelial gaping of the wound, misalignment of the roof and floor of the incision on the endothelial side, Descemet’s membrane detachment and loss of coaptation along the stromal tunnel[10-12]. In our study, the OCT-analysis of the morphological features of the CCI showed that the stress of an implantation through a 1.4 mm CCI is not associated with any particular morphological changes or intraoperative complications. The implantation of the new MJ14 Incise® IOL through a 1.4 mm incision requires a wound-assisted technique that leads to increased pressure in the anterior chamber with viscoelastic leakage. A correct injection of the IOL needs constant pressure and during the procedure it is important to pay attention to the tilting of the tip of the injector.
As a results of our study, in both groups the CCIs healed fast from the first week of follow-up and only temporary morphological alterations were detectable through anterior segment imaging, with no evidence of any morphological feature at 6 and 18mo. The CCIs in group A presented statistically significant fewer endothelial gapings (P=0.04) and local detachment of Descemet’s membrane (P=0.03) in the first postoperative days than the CCIs in group B; this was probably caused by the smaller incision size at the time of implantation compared to those in group B which underwent an enlargement to 1.8 mm prior to the IOL implant (Figures 3, 4).

Figure 3 Graphic representation of the endothelial gaping of the wound through time in the main CCI for both IOLs.

Figure 4 Graphic representation of the local detachment of Descemet’s membrane in the main CCI for both IOLs.
In group B the enlargement of the main incision, performed using a precalibrated knife, probably created a movement of the margins of the incision causing a major incidence of endothelial gaping. Interestingly, we found very few microstructural alterations in the first days postoperatively and these alterations had disappeared at the 1-month followup. In our experience 1.4 mm incisions are not altered by the surgical trauma caused by the enlargement of the CCI and the wound-assisted injection of the Incise IOL; however, this does not seem to cause any important difference in terms of postoperative BCVA between the two groups.
PCO remains one of the most common complications in cataract surgery. Many studies have tried to investigate the factors influencing its development[18-21] and IOL design is one of them[22]. Moreover, the introduction of sharp optic edges appears to be effective in order to reach lower PCO incidence.In particular the new Incise® MJ14 IOL has a new square-edge of 5 µm for 360° with an acute angle[13]. In our study PCO score was low in both groups with better results in the Incise®MJ14 IOL group implantation. It is still unclear whether differences in the style of IOL haptics play a role in PCO inhibition. However, our results show a low rate of PCO which only occurred at the 18mo follow-up. The capsular opacity involved only the edge and peripheral areas of the optic plate with a very low PCO score. Despite the peripheral opacity,there was no influence on the final BCVA of the patients at the 18mo follow-up.
In conclusion, both techniques appear to be safe and effective with rapid visual recovery and high patient satisfaction.B-MICS associated with Incise® MJ14 IOL implantation through a 1.4 mm incision is a minimally invasive technique with fast corneal healing, a very low rate of CCI morphological changes and PCO incidence in the long-term follow-up. The new Incise® IOL makes the B-MICS technique more complete since it is no longer necessary to enlarge microincisions;this was its principal limitation when carrying out bimanual cataract surgery.
ACKNOWLEDGEMENTS
Preliminary results of this study have been presented at XXXIII Congress of the ESCRS 5-9 September 2015 in Barcelona.
Conflicts of Interest: Cavallini GM, None; Verdina T, None;De Maria M, None; Fornasari E, None; Torlai G, None;Volante V, None; Donati S, None; Cagini C, None.
REFERENCES
1 Dick HB. Controlled clinical trial comparing biaxial microincision with coaxial small incision for cataract surgery. Eur J Ophthalmol 2012;22(5):739-750.
2 Cavallini GM, Campi L, Torlai G, Forlini M, Fornasari E. Clear corneal incisions in bimanual microincision cataract surgery: long-term woundhealing architecture. J Cataract Refract Surg 2012;38(10):1743-1748.
3 Cavallini GM, Campi L, Masini C, Pelloni S, Pupino A. Bimanual microphacoemulsification versus coaxial miniphacoemulsification:prospective study. J Cataract Refract Surg 2007;33(3):387-392.
4 Cavallini GM, Volante V, Verdina T, Forlini M, Bigliardi MC, De Maria M, Torlai G, Delvecchio G. Results and complications of surgeons-intraining learning bimanual microincision cataract surgery. J Cataract Refract Surg 2015;41(1):105-115.
5 Aliò JL, Rodriguez-Prats JL, Galal A. Advances in microincision cataract surgery intraocular lenses. Curr Opin Ophthalmol 2006;17(1):80-93.
6 Kurz S, Krummenauer F, Gabriel P, Pfeiffer N, Dick HB. Biaxial microincision versus coaxial small-incision clear cornea cataract surgery.Ophthalmology 2006;113(10):1818-1826.
7 Tetikoğlu M, Yeter C, Helvacıoğlu F, Aktaş S, Sağdık HM, Özcura F. Effect of corneal incision enlargement on surgically induced astigmatism in biaxial microincision cataract surgery. Turk J Ophthalmol 2016;46(3):99-103.
8 Tetz MR, Auffarth GU, Sperker M, Blum M, Völcker HE. Photographic image analysis system of posterior capsule opacification. J Cataract Refract Surg 1997;23(10):1515-1520.
9 Calladine D, Packard R. Clear corneal incision architecture in the immediate postoperative period evaluated using optical coherence tomography. J Cataract Refract Surg 2007;33(8):1429-1435.
10 Müller M, Kohnen T. Incisions for biaxial and coaxial microincision cataract surgery. Ophthalmologe 2010;107(2):108-115.
11 Teixeira A, Salaroli C, Filho FR, Pinto FT, Souza N, Sousa BA,Allemann N. Architectural analysis of clear corneal incision techniques in cataract surgery using Fourier-domain OCT. Ophthalmic Surg Lasers Imaging 2012;43(6 Suppl):S103-S108.
12 Xia Y, Liu X, Luo L, Zeng Y, Cai X, Zeng M, Liu Y. Early changes in clear cornea incision after phacoemulsification: an anterior segment optical coherence tomography study. Acta Ophthalmol 2009;87(7):764-768.
13 Von Sonnleithner C, Bergholz R, Ginnermann J, Klamann MK,Torun N, Bertelmann E. Clinical results and higher-order aberrations after 1.4-mm biaxial cataract surgery and implantation of a new aspheric intraocular lens. Ophthalmic Res 2015;53(1):8-14.
14 Cavallini GM, Verdina T, Forlini M, Volante V, De Maria M, Torlai G,Benatti C, Delvecchio G. Long-term follow-up for bimanual microincision cataract surgery: comparison of results obtained by surgeons in training and experienced surgeons. Clin Ophthalmol 2016;10:979-987.
15 Al Mahmood AM, Al-Swailem SA, Behrens A. Clear corneal incision in cataract surgery. Middle East Afr J Ophthalmol 2014;21(1):25-31.
16 Fukuda S, Kawana K, Yasuno Y, Oshika T. Wound architecture of clear corneal incision with or without stromal hydration observed with 3-dimensional optical coherence tomography. Am J Ophthalmol 2011;151(3):413-419.
17 Tong AY, Gupta PK, Kim T. Wound closure and tissue adhesives in clear corneal incision cataract surgery. Curr Opin Ophthalmol 2017.[Epub ahead of print]
18 Cavallini GM, Masini C, Campi L, Pelloni S. Capsulorhexis phimosis after bimanual microphacoemulsification and in-the-bag implantation of the Akreos MI60 intraocular lens. J Cataract Refract Surg 2008;34(9):1598-1600.
19 Svancarova R, Novak J, Adamkova H. The influence of lens capsule mechanical polishing to the secondary cataract development. Cesk Slov Oftalmol 2010;66(1):21-25.
20 Marcantonio JM, Vrensen GF. Cell biology of posterior capsular opacification. Eye (Lond) 1999;13(Pt 3b):484-488.
21 Awasthi N, Guo S, Wagner BJ. Posterior capsular opacification: a problem reduced but not yet eradicated. Arch Ophthalmol 2009;127(4):555-562.
22 Findl O, Buehl W, Bauer P, Sycha T. Interventions for preventing posterior capsule opacification. Cochrane Database Syst Rev 2010;2:CD003738.