Dear Editor,
Evidence of oculomotor nerve (ON) synkinesis is a common occurrence following both acquired and congenital III nerve palsy[1]. It is generally accepted that aberrant regeneration is the likely aetiology of synkinesis in acquired III nerve palsy, following intracranial aneurysm,trauma, compressive neoplasms, cavernous sinus thrombosis and basilar meningitis[2].
In 1935, Bielschowsky[3] hypothesized that oculomotor synkinesis was caused by axonal misdirection. Since then, alternative theories have been posited to explain this phenomenon, such as central nuclear reorganization, ephaptic transmission and denervation supersensitivity[1-2]. Following histopathologic, clinical and experimental evidence, random misdirection of regenerating motor axons nowadays still represents the most accepted explanation of the synkinetic phenomena[1,4]. Two mechanisms have been suggested to explain this: a misdirection of regenerating nerve fibres at the lesion site and collateral sprouting of uninjured neurons in the ON nuclei to replace damaged axons[1,4-7].
An 86-year-old woman presented with a history of isolated severe ptosis of the left upper eyelid since one year (Figure 1A).She had no other symptoms and her medical history was unremarkable. On clinical examination, she presented an ON palsy. The palpebral fissure measured 9 mm on the right and 1 mm on the left. No mechanical causes for the ptosis such as swelling, palpable mass or subtarsal abnormalities were observed. A complete resolution of the ptosis was underlined when the patients voluntarily closed or squeezed the fellow eye, achieving a 9-mm palpebral fissure (Figure 1B).
Pupils light reflexes were normal and a mild anisocoria (2.5 mm)was found. Her best-corrected visual acuity was 8/10 in both eyes. Referred to an ophthalmologist, the biomicroscopic exam did not reveal any anomaly and even the intraocular pressure was in range. Exophthalmometry measurements were normal and symmetric. Pseudoptosis was excluded. Due to the ptosis,orthoptic assessment (including Hess chart and cover test)could be performed only with mechanical elevation of the lid;it revealed a superior rectus (SR) palsy in the left eye. Patient’s blood analysis were within the normal limits.
The patient missed the succeeding follow-ups and presented one year later. The ptosis was nearly resolved and a light levator palpebrae superior (LPS) contraction was still observed when the patient closed the right eye (Figure 2). Patient denied any surgery or medical treatment since the last visit and reported a self-resolution of the ptosis. Pupils reflexes were normal and the palpebral fissure measured 9 mm and 7 mm on right and left eye respectively.
Cranial magnetic resonance imaging (MRI) was performed,revealing a neurovascular conflict between the ON and posterior cerebral artery (PCA) (Figure 3A). A second MRI,evaluated by the same operator, revealed that the neurovascular conflict was no longer traceable (Figure 3B). Orthoptic assessment showed a mild improvement of the left SR palsy and a compensation of the right eye with the hyperfunction of the inferior rectus (IR).
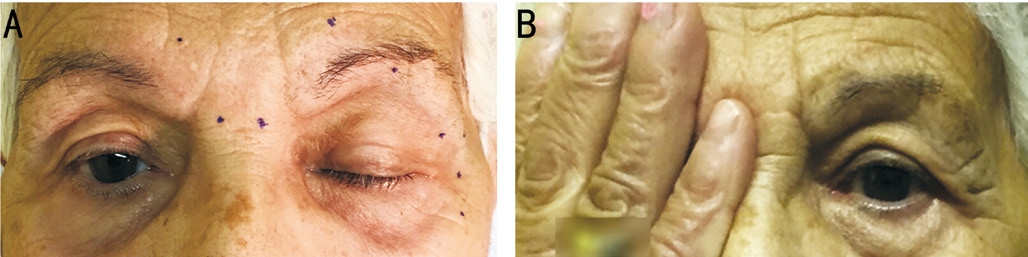
Figure 1 Pictures of the clinic case A: Patient presented with a severe unilateral ptosis of the left upper eyelid, 1 mm palpebral aperture in primary gaze; B: The ptosis resolved when the contralateral eye was closed; in this condition the palpebral aperture measured 9 mm.

Figure 2 Patient presented after one year and the ptosis was nearly resolved.
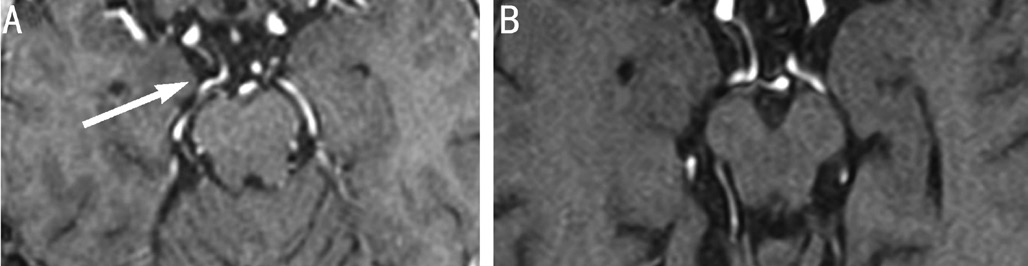
Figure 3 Axial T1-weighted 3D MRI of patient A: Cranial MRI revealed a neurovascular conflict (white arrow) between ON and PCA; B:After one year the neurovascular conflict was no longer traceable.
Since other causes of ptosis were excluded (medical history and orthoptic assessment), and basing on the imaging findings,we supposed that in the present case, nervous impulses to muscles normally innervated by the facial nerve (FN) are accompanied by contraction of muscles usually innervated by the ON.
In order to explain a possible synkinesis between ON and FN,it is necessary to analyze the topographic relationship between the two nerves and their motor nuclei. The motor neurons of the ON originate from the midbrain[6]. The neurons of the extraocular muscles are arranged bilaterally in longitudinal groups. A midline structure called central caudal nucleus(CCN), is the only unpaired nucleus and supplies the LPS muscle of both sides[6-9].
Myelinated axons leave the oculomotor nuclei and pass ventral to the interpeduncular fossa moving below the PCA. These fibers do not combine with the ON, instead they merely travel within its sheath (Figure 4). The fibers reach the orbit through the superior orbital fissure[1,6].
The nuclei of origin of the FN lie in the tegmentum rhombencephali and its nuclear complex consists of three different units, the motor nucleus, the nucleus solitarious and the superior salivatory nucleus. The most rostral is the main motor nucleus whose upper part supplies innervation to the forehead muscles and orbicularis oculi (OO) muscle. The fibres bundles of the motor neurons loop over the abducent nucleus,reaching the surface of the brain in the angle between pons and cerebellum[1,6].
During their infranuclear intracranial and extracranial course,there are no direct connections between fibres of the ON and the FN are known to exist. Also, during the extracranial course there is no close relationship between fibers of the ON and FN cranial nerves.
One of the main causes of sudden onset, unilateral third nerve palsy is the ON compression from an aneurysm at the junction of the posterior communicating and internal carotid arteries[3,10-14]. In our case, MRI revealed the presence of a vascular compression of the ON by the PCA (Figure 3A).Third nerve paresis has already been reported to be caused by vascular compression by the PCA without aneurysms in four cases[10-12,14] and by the basilar artery in another one[15].
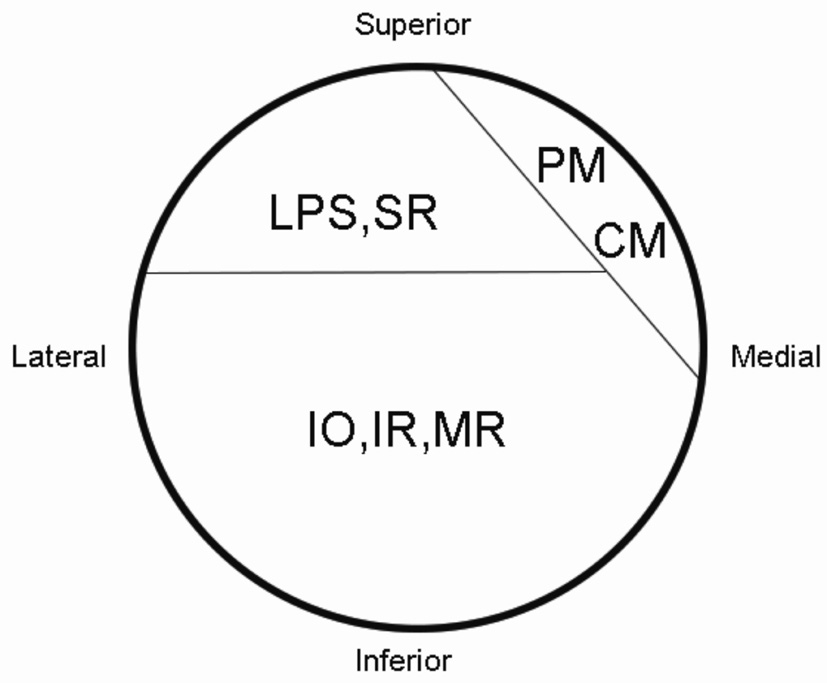
Figure 4 The cross-section of ON in subarachnoid space shows topographical distribution of nervous fibers The superior division contains axons to LPS muscle and SR; the inferior division contains axons to the medial rectus (MR), IR and inferior oblique (IO); the PM and ciliary muscle (CM) axons are present in the dorsomedial quadrant of the nerve.
In this case, the PCA impinged on the ON in its subarachnoid portion on a dorsomedial direction, compressing the axons for the LPS and the pupillary muscle (PM), according to the anatomical disposition of motor fibers in the nerve (Figure 4). Indeed the patient presented with anisocoria and nearly complete ptosis of the left eye. These findings resolved when the contralateral eye was closed, evoking the presence of a concomitant synkinesis between ON and FN, the voluntary contraction of the right OO elicit an aberrant stimulus to the contralateal LPS, inducing a simultaneous elevation of the contralateral upper eyelid. In case of synkinesis, certain muscle groups are innervated by cranial nerve fibres which are normally destined for other muscles. A variety of theories have been proposed to explain the synkinesis, including ephaptic transmission and central/nuclear synaptic reorganisation[1-4]. However is generally accepted that aberrant regeneration is the likely aetiology of synkinesis in ON palsy and two mechanisms have been suggested: a misdirection of regenerating nerve fibers at the lesion site and collateral sprouting of uninjured neurons in the nerve nuclei to replace damaged axons. As during the extracranial course there is no close relationship between fibers of the ON and FN, it is probable that the vascular compression induced a rearrange of the neuronal connection at a level of the nerves nuclei,according to the latter mechanism. Rare cases of synkinesis between ON and FN fibers have been already reported and it has been hypothesized that aberrant regeneration develop in the midbrain at the level of the superior colliculi, where the midline unpaired CCN is located as the most caudal part of the oculomotor nuclear complex[2,6]. Since the motor nuclei of the FN lie more caudal, nerve sprouts would emerged above the nucleus. Lemke and el Bably[6] reported a case of a young man suffering from a facial-oculomotor synkinesis, a unilateral elevation of the ptotic eyelid appeared with the contraction of the platysma. Brandley and Toone[8], Kirkham[16] described two cases with improvement of the ptosis during smiling.
Moreover after one year the ptosis nearly resolved, but a light LPS contraction was still observed when the patient closed the right eye. A second MRI revealed that the neurovascular conflict was no longer traceable (Figure 3B). The disappear of the ptosis after the apparent resolution of the neurovascular syndrome, made our hypothesis a likely explanation for the synkinetic movements observed. As the ON did not suffer more because of the PCA compression, the LPS recovery was surprisingly rapid. Reversibility has already been documented in at least two cases of acquired oculomotor synkinesis[7,17] and Nakagawa et al[10] reported a case of peripheral ON paresis due to compression by the PCA, which was successfully treated by microvascular decompression. Despite the resolution of ON palsy, aberrant innervation between LPS and OO was still present during right eye close, even if less manifest, as fibers reorganization at a central nuclei level seemed to be unlikely reversible. This is the first description of an acquired unilateral blepharoptosis of the upper eyelid resolving by controlateral eye closing, underlying an ON peripheral palsy and plausible synkinesis with FN. To our knowledge, a clearly proven mechanism responsible for the acquired contralateral FN synkinesis observed in our patient is unknown. The theory of aberrant regeneration underlying a rearrangement of the neuronal connection seems plausible.
ACKNOWLEDGEMENTS
The patient signed a written informed consent and provided consent for the publication of this case.
Conflicts of Interest: Tarallo M, None; Gharbiya M, None;Onesti MG, None; Conversi A, None; Toscani M, None;Fino P, None; Scuderi N, None; Di Taranto G, None.
REFERENCES
1 Shuttleworth GN, Steel DH, Silverman BW, Harrad RA. Patterns of III nerve synkinesis. Strabismus 1998;6(4):181-190.
2 Sibony PA, Lessell S, Gittinger JW Jr. Acquired oculomotor synkinesis.Surv Ophthalmol 1984;28(5):382-390.
3 Bielschowsky A. Lectures on motor anomalies of the eyes: II. Paralysis of individual eye muscles. Arch Ophthalmol 1935;13(1):33-59.
4 Sibony PA, Evinger C, Lessell S. Retrograde horseradish peroxidase transport after oculomotor nerve injury. Invest Ophthalmol Vis Sci 1986;27(6):975-980.
5 Guy J, Engel HM, Lessner AM. Acquired contralateral oculomotor synkinesis. Arch Neurol 1989;46(9):1021-1023.
6 Lemke C, el Bably I. Synkinesis between facial nerve and oculomotor nerve. A case report. Ann Anat 1998;180(4):339-342.
7 Buckley EG, Ellis FD, Postel E, Saunders T. Posttraumatic abducens to oculomotor nerve misdirection. J AAPOS 2005;9(1):12-16.
8 Bradley WG, Toone KB. Synkinetic movements of the eyelid: a case with some unusual mechanisms of paradoxical lid retraction. J Neurol Neurosurg Psychiatr 1967;30(6):578-579.
9 Büttner-Ennever JA, Büttner U, Cohen B, Baumgartner G. Vertical glaze paralysis and the rostral interstitial nucleus of the medial longitudinal fasciculus. Brain 1982;105(Pt 1):125-149.
10 Nakagawa H, Nakajima S, Nakajima Y, Furuta Y, Nishi O, Nishi K. Bilateral oculomotor nerve palsies due to posterior cerebral arterial compression relieved by microvascular decompression--case report.Neurol Med Chir (Tokyo) 1991;31(1):45-48.
11 Mulderink TA, Bendok BR, Yapor WY, Batjer HH. Third nerve paresis caused by vascular compression by the posterior communicating artery. J Stroke Cerebrovasc Dis 2001;10(3):139-141.
12 Silva Jr EB, Ramina R, Meneses MS, Kowacs PA, Silva EB. Bilateral oculomotor nerve palsies due to vascular conflict. Arq Neuropsiquiatr 2010;68(5):819-821.
13 Esmer AF, Sen T, Comert A, Tuccar E, Karahan ST. The neurovascular relationships of the oculomotor nerve. Clin Anat 2011;24(5):583-589.
14 Jo YS, Kim SK, Kim DH, Kim JH, Na SJ. Complete oculomotor nerve palsy caused by direct compression of the posterior cerebral artery. J Stroke Cerebrovasc Dis 2015;24(7):e189-e190.
15 Hashimoto M, Ohtsuka K, Akiba H, Harada K. Vascular compression of the oculomotor nerve disclosed by thin-slice magnetic resonance imaging. Am J Ophthalmol 1998;125(6):881-882.
16 Kirkham TH. Paradoxical elevation of eyelid on smiling. Am J Ophthalmol 1971;72(1):207-208.
17 Johnson LN, Pack WL. Transient oculomotor nerve misdirection in a case of pituitary tumor with hemorrhage. Case report. Arch Ophthalmol 1988;106(5):584-585.