Dear Editor,
I am Dr. João Beato, from the Ophthalmology Department of Sao João Hospital Center, Porto, Portugal. I write to present a case of combined penetrating keratoplasty (PKP)with temporary Eckardt keratoprosthesis, pars plana vitrectomy(PPV) and Ahmed glaucoma valve (AGV) implantation into the ciliary sulcus in a patient with previous history of open globe injury (OGI).
Eye trauma resulting in an OGI is a leading cause of unilateral visual loss in young patients[1-2]. It represents an important public health problem, with an estimated global incidence of 3.0/100 000 persons per year[2]. The injuries are most frequently caused by sharp objects, followed by blunt mechanisms[1,3]. Domestic accidents related to hobby activities represent the most frequent context of trauma, and men are typically more affected than women[4-6].
Ocular trauma can result in significant visual morbidity. Many of these patients undergo extensive surgical rehabilitation for their OGI[7-10]. Visual recovery after trauma is usually challenging and depends on the nature and extent of the initial lesions[10]. On the other hand, intraocular pressure (IOP)elevation can occur as a direct result of the initial eye injury or secondary to multiple intraocular surgeries[9-11]. The lifelong management, outcome and prognosis of OGI still remain largely unaddressed in the literature[3,5,8-9].
An eight-year-old boy, with no systemic or ocular known disease, was referred to our Emergency Department, in February 1995, because of right eye penetrating trauma with scissors at home. Right eye visual acuity was hand motions and slit-lamp observation revealed an extensive paracentral full-thickness corneal laceration, shallow anterior chamber and traumatic cataract. Left eye examination was unremarkable.He underwent corneal laceration suture at the Operating Room in the Emergency Department. Three weeks later, an extracapsular lens extraction with posterior intraocular lens[Pharmacia 722C® poly (methyl methacrylate) IOL, Groningen BV, The Netherlands - power +24.0 diopters] implantation in the bag was performed. Best corrected visual acuity (BCVA)one month after surgery was 20/30 with a manifest refraction of -2.00 -3.00 ×40°.
The patient was followed at the Ophthalmology Outpatient Clinic, and in March 2000, five years after the traumatism,IOP raised to 25 mm Hg and anterior peripheral synechia were visible at this time on gonioscopy. He was treated with a fixed combination of timolol maleate 5 mg/mL and dorzolamide hydrochloride 20 mg/mL, with good tolerance and adequate IOP control. At the beginning of 2008, BCVA dropped to 20/100 and IOP increased to 30 mm Hg. Biomicroscopy showed an anterior subluxation of the capsular bag-IOL complex with pigment dispersion on corneal endothelium and a vertical cup-to-disc of 0.6 was observed on fundoscopy.Brimonidine tartrate 1% and latanoprost 50 µm/mL were additionally prescribed for IOP control. In November 2009,due to uncontrolled ocular hypertension (OHT) the patient underwent surgical removal of the subluxated capsular bag-IOL complex with anterior vitrectomy and implantation of a retroiridian Artisan® (Ophtec B.V., Groningen, The Netherlands), power +20.0 diopters. In the postoperative period, IOP was not controlled with medical therapy and a trabeculectomy with 5-fluorouracil was performed in January 2010.
In March 2011, one year after trabeculectomy, BCVA was hand motions; IOP was 16 mm Hg with maximum tolerated hypotensive therapy and fundoscopy showed a glaucomatous optic disc with vertical cup-to-disc of 0.9. A sensorial small angle exotropia developed.
Later, in April 2013, ophthalmologic examination showed a bullous keratopathy with retroiridian lens subluxation and IOP of 24 mm Hg (Figure 1). Therefore, we decided to perform a combined PKP with Eckardt temporary keratoprosthesis®(Heinrich Woehlk Kontaktlinsen, Kiel, Germany), retroiridian lens extraction, PPV and Ahmed® glaucoma valve, AGV FP7 model (New World Medical, Rancho Cucamonga, CA, USA)implantation in the right eye under general anesthesia. Three different surgeons performed the surgery. First, we implanted the plate of the AGV in the superotemporal quadrant; the 23G vitrectomy trocars were then inserted. A temporary Eckardt keratoprosthesis (4 cardinal sutures with 10-0 nylon) was placed after patient’s cornea trephination (7 mm diameter)and removal of the retroiridian Artisan. Complete PPV was then performed in order to allow implantation of the AGV tube into the ciliary sulcus. Later, we sutured the sclerotomies but the infusion cannula remained to provide ocular tonus.The AGV tube was introduced into the ciliary sulcus, through a scleral tunnel done with a 23G needle, and covered with Tutopatch® 5×5 mm2 (Tutogen Medical GmbH, Neunkirchen am Brand, Germany) after fixation to scleral wall with 10-0 nylon. Conjunctiva was sutured to the limbus with 8-0 nylon sutures. The Eckardt keratoprosthesis was then removed and the corneal graft (7.25 mm diameter) was placed and sutured with sixteen interrupted 10-0 nylon sutures under a low fluid infusion pressure of 5 mm Hg. Finally, the infusion cannula was removed and the sclerotomy closed. On the first day after surgery, corneal graft was transparent and the tube was properly placed in the sulcus (Figure 2). At the 12mo postoperative visit, BCVA was 20/200 and IOP was 15 mm Hg with no hypotensive medication (Figure 3).
In the present case report, we emphasize the importance of long-term follow-up in patients with OGI. Also, we show that a multidisciplinary approach may be mandatory for surgical rehabilitation of these eyes.
Ocular trauma remains a subject of controversies and the strategies for optimal management of OGIs are still under debate[12]. Surgical outcomes of injured eyes have been reported with diverse success rates[4,10]. Previous studies demonstrate that eyes requiring multiple procedures were found to have an overall worse postoperative visual acuity[10] and also higher rates of OHT and glaucoma[9]. Older age, lens damage,need for PKP were also identified as important risk factors for worse functional outcomes[4-5,9,11]. In our patient, ocular injury occurred in childhood and we were able to recover vision and control IOP for several years. However, in the long run, complications in the anterior segment, in particular,anterior peripheral synechiae with IOP increase, capsular bag-IOL subluxation with pigment dispersion and corneal decompensation lead to further surgeries.
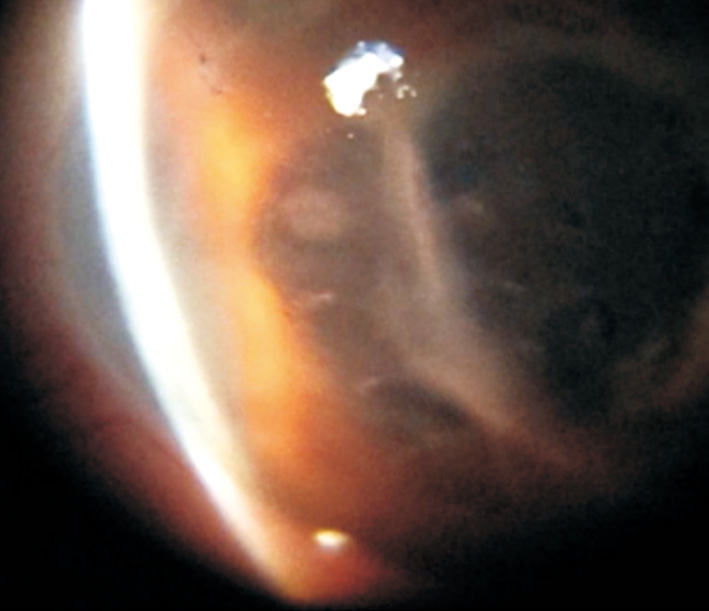
Figure 1 Right eye bullous keratopathy (April 2013).
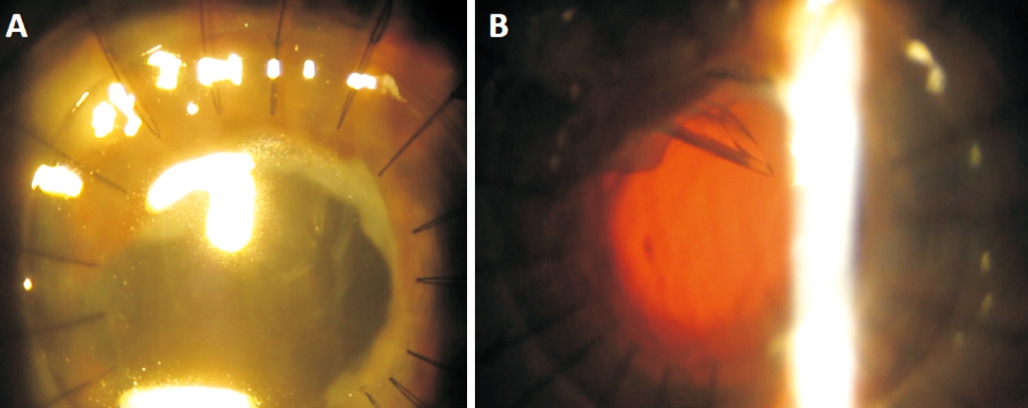
Figure 2 First day after surgery A: Transparent corneal graft; B:Ahmed valve tube in the ciliary sulcus.
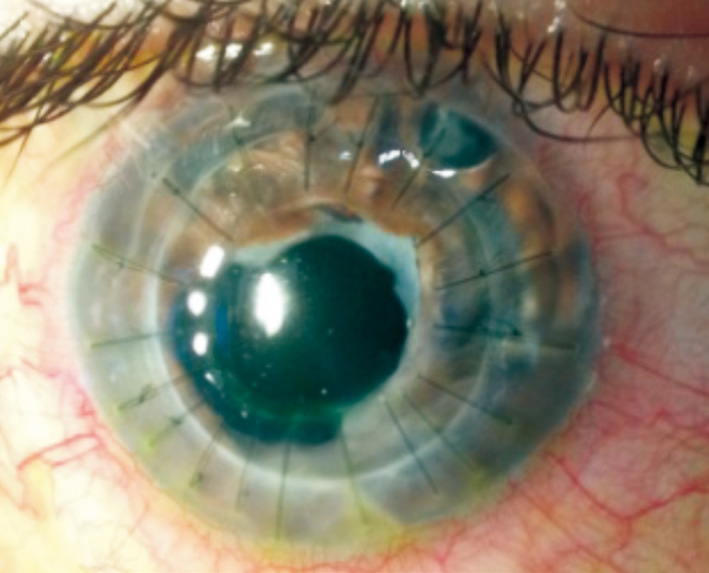
Figure 3 Slit-lamp examination one year after combined surgery.
In a study regarding OGI outcomes, Turalba et al[9] found that 12% of the patients required glaucoma surgery and all of them had between 1 and 3 previous intraocular surgeries (including open globe repair). Most of the patients underwent surgery within the first 6mo and only 3 patients needed glaucoma surgery >2y after the injury. Chronic angle closure glaucoma was often the indication for glaucoma surgery performed more than a year after an OGI showing the importance of life-long follow-up in these patients[9]. In our case, the development of anterior peripheral synechiae and, later, pigment dispersion,lead to an IOP increase of difficult control with medical therapy. Moreover, intraocular inflammation associated with the multiple surgeries might have contributed to the IOP rise.Corneal endothelium is another concern in these eyes.Multiple surgeries contribute to endothelial failure and PKP is frequently needed[9,11]. Although PKP is often associated with an increased risk of OHT and secondary graft failure,preserving ambulatory vision is frequently possible[13].
In our patient, eighteen years and four ocular surgeries later, a bullous keratopathy developed and IOP increased again despite maximum tolerated hypotensive topical therapy. As it would not be possible to rehabilitate this eye with a single procedure,we decided to perform a multidisciplinary approach in order to provide long-term IOP control and corneal transparency.Although this combined approach implied a significantly increased risk of complications, such as intraoperative choroidal hemorrhage, it allowed us to address all the problems (bullous keratopathy, retroiridian lens subluxation and uncontrolled OHT) in a single episode of anesthesia, with faster patient’s recovery.
AGV was our choice for IOP control; however, a cyclodestructive procedure could have been used. Vitrectomy allowed us to place the AGV tube into ciliary sulcus, which seems to improve safety regarding corneal endothelium[14] but with the same effectiveness of anterior chamber AGV implantation[15].Temporary Eckardt keratoprosthesis[16] was a valuable option that allowed PPV and insertion of AGV tube into ciliary sulcus. It was rather challenging to perform a scleral tunnel for the AGV tube, since the interface between Eckardt keratoprosthesis® and patient’s cornea was not completely leakproof. The placement of donor cornea at the end of the surgery, under a low fluid infusion pressure, aimed to preserve its endothelium; however it was difficult to suture the graft because the patient was aphakic with low ocular tonus.
To our knowledge, there have been no reported cases with PPV, AGV and PKP with temporary Eckardt keratoprosthesis performed at the same intervention. According to our experience and literature data, placement of the Ahmed valve in conjunction with PKP may be a safe and effective procedure in the short term[17]. The placement of the tube into the ciliary sulcus and vitrectomy may reduce the likelihood of graft decompensation.
ACKNOWLEDGEMENTS
Meeting presentations: “1st European Meeting of Young Ophthalmologists”, Porto, Portugal, July 11-12th 2014.
Conflicts of Interest: Beato J, None; Melo AB, None; Faria PA, None; Torrão L, None; Falcão-Reis F, None.
REFERENCES
1 Sternberg P Jr, de Juan E Jr, Michels RG. Penetrating ocular injuries in young patients. Initial injuries and visual results. Retina 1984;4(1):5-8.
2 Schrader WF. Epidemiology of open globe eye injuries: analysis of 1026 cases in 18 years. Klin Monbl Augenheilkd 2004;221(8):629-635.
3 Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye (Lond) 2006;20(12):1336-1341.
4 Teixeira SM, Bastos RR, Falcão MS, Falcão-Reis FM, Rocha-Sousa AA.Open-globe injuries at an emergency department in Porto, Portugal:clinical features and prognostic factors. Eur J Ophthalmol 2014;24(6):932-939.
5 Girkin CA, McGwin G Jr, Morris R, Kuhn F. Glaucoma following penetrating ocular trauma: a cohort study of the United States Eye Injury Registry. Am J Ophthalmol 2005;139(1):100-105.
6 Falcão M, Camisa E, Falcão-Reis F. Characteristics of open-globe injuries in northwestern Portugal. Ophthalmologica 2010;224(6):389-394.
7 De Leon-Ortega JE, Girkin CA. Ocular trauma-related glaucoma.Ophthalmol Clin North Am 2002;15(2):215-223.
8 Bai HQ, Yao L, Wang DB, Jin R, Wang YX. Causes and treatments of traumatic secondary glaucoma. Eur J Ophthalmol 2009;19(2):201-206.
9 Turalba AV, Shah AS, Andreoli MT, Andreoli CM, Rhee DJ. Predictors and outcomes of ocular hypertension after open-globe injury. J Glaucoma 2014;23(1):5-10.
10 Andreoli MT, Andreoli CM. Surgical rehabilitation of the open globe injury patient. Am J Ophthalmol 2012;153(5):856-860.
11 Bojikian KD, Stein AL, Slabaugh MA, Chen PP. Incidence and risk factors for traumatic intraocular pressure elevation and traumatic glaucoma after open-globe injury. Eye (Lond) 2015;29(12):1579-1584.
12 Agrawal R, Shah M, Mireskandari K, Yong GK. Controversies in ocular trauma classification and management: review. Int Ophthalmol 2013;33(4):435-445.
13 Suleiman Y, Amm M, Duncker GI, Nölle B. Prognosis of corneal transplantation after penetrating eye injury. Klin Monbl Augenheilkd 2004;221(8):658-673.
14 Seo JW, Lee JY, Nam DH, Lee DY. Comparison of the changes in corneal endothelial cells after pars plana and anterior chamber ahmed valve implant. J Ophthalmol 2015;2015:486832.
15 Maris PJ Jr, Tsai JC, Khatib N, Bansal R, Al-Aswad LA. Clinical outcomes of Ahmed glaucoma valve in posterior segment versus anterior chamber. J Glaucoma 2013;22(3):183-189.
16 Eckardt C. A new temporary keratoprosthesis. Klin Monbl Augenheilkd 1987;191(3):243.
17 Knape RM, Szymarek TN, Tuli SS, Driebe WT, Sherwood MB, Smith MF. Five-year outcomes of eyes with glaucoma drainage device and penetrating keratoplasty. J Glaucoma 2012;21(9):608-614.