·
·Clinical Research·Current
Issue· ·Achieve· ·Search Articles· ·Online
Submission· ·About IJO· PMC
Evaluation of visual quality of
spherical and aspherical intraocular lenses by Optical Quality Analysis System
Yan Chen1, Xue Wang1, Chuan-Di Zhou2,
Qiang Wu1
1Department of Ophthalmology,
Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai
200233, China
2Department of
Ophthalmology, Shanghai Jiao Tong University Affiliated First People’s
Hospital, Shanghai 200080, China
Correspondence
to: Qiang
Wu. Department of Ophthalmology, Shanghai Jiao Tong University Affiliated Sixth
People’s Hospital, Shanghai 200233, China. eyedoctor07@outlook.com
Received:
2016-11-20
Accepted: 2017-01-20
Abstract
AIM: To evaluate the
impact of spherical and aspherical intraocular lenses on the postoperative
visual quality of age-related cataract patients using Optical Quality Analysis
System (OQAS).
METHODS: Seventy-four
eyes with age-related cataracts
were randomly divided into spherical and aspherical lens implantation groups. Best-corrected visual
acuity (BCVA) was measured preoperatively,
one day, one week, two weeks,
one month and two
months after surgery. A biometric systems analysis using the OQAS objective
scattering index (OSI)
was performed.
RESULTS: There were no significant differences in visual
acuity (P>0.05) before and after spherical and aspheric
lens implantation. There was a negative linear
correction between the OSI value and BCVA (r=-0.634, P=0.000),
and positive corrections between the OSI value and the lens LOCUS III value of
nucleus color (NC), nucleus opacity (NO), cortex (C) and posterior lens
capsular (P) (r=0.704, P=0.000; r=0.514, P=0.000;
r=0.276, P=0.020; r=0.417, P=0.000, respectively).
OSI values of spherical vs
aspherical lenses were 11.5±3.6 vs
11.8±3.4, 4.1±0.9 vs 3.3±0.8, 3.5±0.9 vs 2.7±0.7, 3.3±0.8 vs
2.6±0.7, 3.2±0.7 vs 2.5±0.8, and 3.2±0.8 vs
2.5±0.8 before and 1d, 1, 2wk, 1 and 2mo
after surgery, respectively. All time points varied
significantly (P<0.01) between the two groups.
CONCLUSION: Aspherical IOLs does not significantly affect visual acuity compared with spherical IOLs. The OSI value, was
significantly lower in the aspherical lens group
compared with the spherical lens. This study shows that objective visual
quality of aspheric IOLs is better than
that of the spherical lens by
means of OQAS biological measurement method.
KEYWORDS: optical quality analysis
system; age-related cataract; spherical
lens; aspherical lens;
objective scattering index
DOI:10.18240/ijo.2017.06.13
Citation: Chen Y,
Wang X, Zhou CD, Wu Q. Evaluation of visual quality of spherical and aspherical
intraocular lenses by Optical Quality Analysis System. Int J Ophthalmol
2017;10(6):914-918
Article
Outline
INTRODUCTION
Cataract
surgery using phacoemulsification and implantation of an intraocular lens (IOL)
is a safe and effective operative intervention[1].
The goal of cataract surgery is not only to restore visual acuity but also to
provide the best possible quality of vision. Aspherical IOLs were created to
compensate for the spherical aberration of the cornea and to lessen total
ocular spherical aberration by IOL implantation[2-4]. Several studies have compared aspheric with spherical
IOLs during the past decades[5-11].
So far, the postoperative visual evaluation has been determined only on the
basis of visual acuity, contrast sensitivity, or higher order aberrations.
There are some controversial viewpoints about the optical quality of aspheric
and spherical IOLs[8-11]. With
the instructions available today, it is possible to study more precisely the
optical quality difference between these two kinds of IOLs.
The Optical
Quality Analysis System (OQAS) is a double-pass based instrument that
clinically measures objective optical quality[12-18]. This system performs the measurements by analyzing
the retinal image of a point source of light obtained after the focalization of
a beam. It has been shown that the OQAS system provided repeatable and accurate
measurements of the optical quality of the eye[12-18].
The aim of our
study is to compare the optical quality of aspheric and
spherical lens implantation using OQAS measurement. This study is the
first time to compare the visual quality of aspheric and
spherical lens implantation using OQAS.
SUBJECTS AND METHODS
Subjects Thirty-eight consecutive Chinese
patients (74 eyes) with age-related cataracts were enrolled from the Department
of Ophthalmology, Sixth Peoples’ Hospital Affiliated of Shanghai Jiaotong
University. This study was approved by the Ethics Committee of the Sixth
Peoples’ Hospital Affiliated of Shanghai Jiaotong University, Shanghai, China.
Written informed consent was obtained from all patients. The patients were
randomly divided into two groups using a random number table. The patients
underwent phacoemulsification and implantation of posterior chamber intraocular
spherical IOLs (AR40) for 37 eyes and aspherical IOLs (ZA9003) for the other 37
eyes, respectively. The mean age of the patients was 69.3±8.2y (range 50-85y).
Inclusion criteria were normal eye pressure, transparent central cornea, normal
fundus examination, and at least 1600 endothelial cells per mm2 in
the central cornea. Patients with a cataract other than a nuclear or
corticonuclear cataract, with history of eye surgery, or with active ocular
pathology were excluded from the study.
Patient
Examinations All patients performed a
thorough eye examination including best-corrected visual acuity (BCVA) and
slit-lamp microscope (SuZhou 66 Co. Ltd., China). Preoperative BCVA was
measured by Snellen charts. The visual acuity of counting fingers and hand
motions were assigned values of 1/200 and 1/400, respectively. The
postoperative BCVA of patients at 1, 2wk, 1 and 2mo was measured in the same
manner as pre-operative BCVA. All cataracts were graded using the Lens
Opacities Classification System III (LOCSIII).
Surgical
Operation All surgeries were
operated by the same skilled surgeon (Wu Q), and the patients were examined by
an researcher (Chen Y). The pupil was dilated with 0.5% tropicamide drops
(Santen, Osaka, Japan) 30min prior to surgery, and the other eye was treated
with a miotic drug to avoid glaucoma attack. Phacoemulsification was performed
under topical anesthesia using 2% lidocaine (ALCON Co. Ltd., USA). The incision
was performed at the 9 o’clock (right eye) or 2 o’clock (left eye) positions of
the cornea. The chamber was injected using Viscoat immediately (SA
Alcon-Couvreur NV, Rijksweg, Puurs, Belgium). Using continuous curvilinear
capsulorhexis, the nucleus was removed using a “stop and chop” skill. An
automated irrigation/aspiration instrument was introduced into the anterior
chamber to remove the cortical remnants and to polish the posterior lens
capsule (ACCURUS600DS, ALCON Co. Ltd., USA). The IOL was placed in the capsular
bag.
Optical Quality
Evaluation We evaluated the optical
quality parameters of the objective scatter index (OSI) using OQAS
(VISIOMTRICS. Inc., Spanish) preoperatively as well as at 1, 2wk, 1 and 2mo
after surgery. The OSI is calculated by measuring the amount of light outside
retinal point spread function (PSF) image in term of the intensity of light in
the center. The refractive error was fully corrected during these evaluations;
the spherical error (up to -8.00 D) was corrected by the OQAS automatically,
and the residual spherical error part (over -8.00 D) and cylindrical error part
were corrected using an external lens. We established by OQAS a 4.0-mm pupil,
and we also ensured that the pupil diameter was more than 4.0 mm in all
subjects. The background illumination was kept at a low level of approximately
25 lx during examination.
Statistical
Analysis All analyses were
performed using SPSS software version 19.0. Wilcoxon rank sum t-tests
were employed for the preoperative and postoperative comparisons and comparisons
between the spherical and aspherical groups of BCVA and lens opacity values.
Single sample t-tests were used to analyze the preoperative comparisons
of OSI values because some values could not be measured due to the severity of
the cataract opacity. Paired sample t-tests were used to analyze the
comparisons of OSI between the two groups at the same time after surgery.
Bivariate correlation models and spearman correlation coefficients were used to
analyze the relationship between OSI and BCVA and the relationship between OSI
and lens opacity values. The results are expressed as the mean±SD, and a value
of P<0.05 was considered statistically significant.
RESULTS
Best-corrected Visual Acuity Before and After Surgery In the spherical IOL group, the mean
BCVA improved at 1d to 0.61±0.16, at 1wk to 0.72±0.16, at 2wk to 0.8±0.15, at
1mo to 0.85±0.12 and at 2mo to 0.85±0.13. In the aspherical IOL group,
the mean BCVA improved at 1d to 0.63±0.13, at 1wk to 0.74±0.15, at 2wk to
0.79±0.12, at 1mo to 0.86±0.12 and at 2mo to 0.87±0.11. There was no difference
between the two groups in BCVA before and after surgery (P>0.05).
Lens Density Before Surgery There are four types of cataract[19]. In the spherical IOL group, the mean nucleus opacity
(NO) value was 2.66±0.96, the mean nucleus color (NC) value was 2.76±1.06, the
mean cortex (C) value was 2.85±0.76, and the mean posterior lens capsular (P)
value was 1.88±1.24. In the aspherical IOL group, the mean NO value was
2.68±0.93, the mean NC value was 2.71±1.13, the mean C value was 2.83±0.89, and
the mean P value was 1.89±1.19. There was no difference in NC, NO, C, and P
between the two groups (P>0.05). These results indicated that
there was no significant difference in the severity of the two groups.
Objective
Scattering Index Values Comparison Between Spherical and
Aspherical Intraocular Lens Figure 1
shows the diagrammatic change of OSI values in one patient in the aspherical
group prior to and at 1d after surgery. The OSI value decreased from 1.8 to
0.8. Figure 2 shows the diagrammatic OSI value trends in the two groups. Table 1 shows the OSI values of the two groups. The
preoperative OSI values of the spherical and aspherical lens groups were 11.5±3.6 and 11.8±3.4,
respectively. There were no significant
differences between the two groups
(P>0.05). OSI values of spherical vs aspherical
lenses were 4.1±0.9 vs 3.3±0.8, 3.5±0.9 vs
2.7±0.7, 3.3±0.8 vs 2.6±0.7, 3.2±0.7 vs 2.5±0.8,
and 3.2±0.8 vs 2.5±0.8 1d,
1, 2wk, 1 and 2mo
after surgery, respectively. There were significant
differences (P<0.01) at all
time points after surgery between the
two groups.
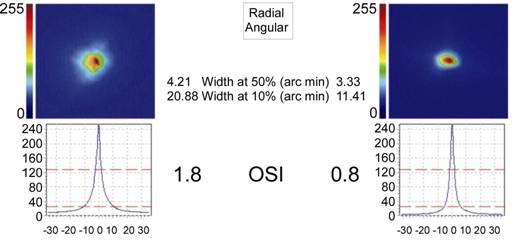
Figure 1 Comparison of OSI change before and after cataract
surgery The OSI value was 1.8
before surgery and 0.8 after surgery.
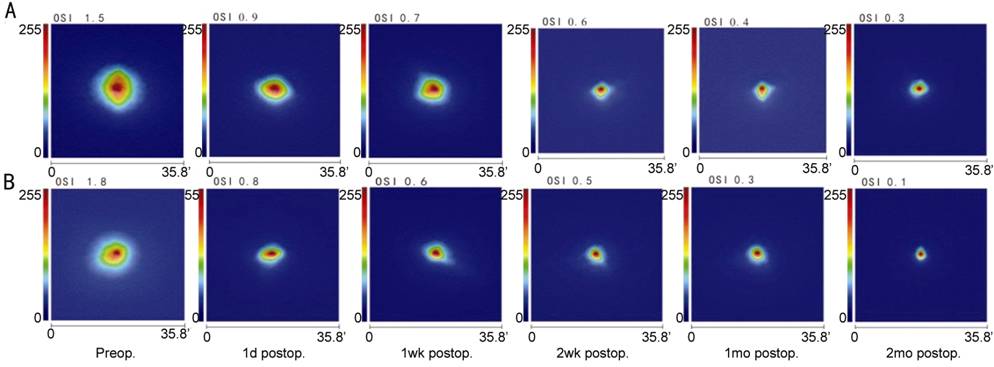
Figure 2
OSI changes with the time A: OSI changes with the
time in the spherical group; B: OSI changes with the time in the aspherical
group. ’An arc minute.
Table 1 OSI
values differences between the two kinds of IOLs mean±SD
|
OSI values |
Spherical IOL |
Aspherical IOL |
|
Preop. |
11.5±3.6 |
11.8±3.4 |
|
1d postop. |
4.1±0.9 |
3.3±0.8a |
|
1wk postop. |
3.5±0.9 |
2.7±0.7a |
|
2wk postop. |
3.3±0.8 |
2.6±0.7a |
|
1mo postop. |
3.2±0.7 |
2.5±0.8a |
|
2mo postop. |
3.2±0.8 |
2.5±0.8a |
IOL: Intraocular
lens; SD: Standard deviation. Comparison of OSI values between aspherical and
spherical IOL at the same time before and after surgery. Values were tested
with paired sample t-test. aP<0.05.
Correction of Objective Scattering Index and Best-corrected Visual
Acuity Preoperatively Figure 3
shows the correlations between the preoperative BCVA and the OSI values of all
of the 74 eyes. There was a negative linear correction between the OSI value
and BCVA (r=-0.634, P=0.000).
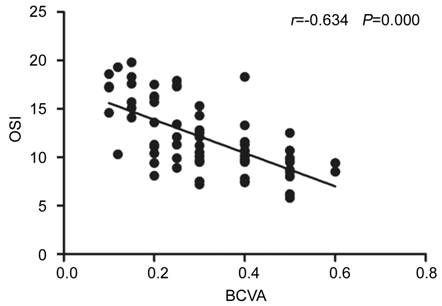
Figure 3
Corrections of BCVA and OSI preoperatively There a negative linear
correction between the OSI value and BCVA (r= -0.634, P=0.000).
Correction of Objective Scattering Index and Lens Density
Preoperatively Figure 4
shows the preoperative positive linear correlations between the lens LOCUS III
value and the OSI value of all the 74 eyes. There were positive linear
correlations between the OSI value and the lens LOCUS III value of nucleus
color (NC), nucleus opacity (NO), cortex (C) and posterior lens capsular (P) (r=0.704,
P=0.000; r=0.514, P=0.000; r=0.276, P=0.020;
r=0.417, P=0.000, respectively).
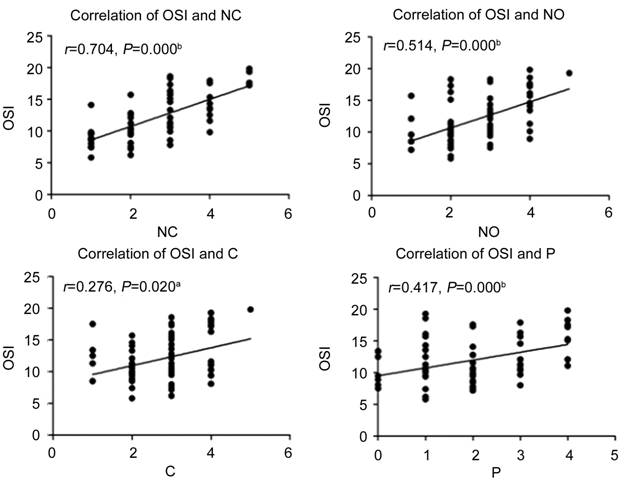
Figure 4 Correction of OSI and lens density preoperatively There were positive
linear correlations between the OSI value and the lens LOCUS III value of nucleus
color (NC), nucleus opacity (NO), cortex (C) and posterior lens capsular (P) (r=0.704,
P=0.000; r=0.514, P=0.000; r=0.276, P=0.020;
r=0.417, P=0.000, respectively). aP<0.05,
bP<0.01.
DISCUSSION
The OQAS was designed in term of the double-pass technique[20], in which the image of a point-source object is
directly recorded after reflection on the retina, and a double pass through the
ocular media has been shown to accurately estimate the eye’s optical quality[12,21]. The OQAS is used to measure OSI,
modulation transfer function threshold (MTF), IOL accommodation, etc.
OSI is a ratio of 12 and 20 points from the
perspective of the annular region of the light and the central 1 point
perspective peak, and it is an important index of optical quality. In the
present study, we evaluated the difference in OSI and its relationship with the
BCVA and LOCUS. We objectively assessed the OSI, and
thereby obtained new reference data for the IOL evaluation.
With the OQAS available, it is possible to study clinically the
correction between the widespread subjective clinical classification for
example BCVA and LOCUS III and the objective methods of quantifying lens
opacification for example OSI. In our study, there was a negative linear
correction between the OSI value and BCVA. and the corrections between OSI and LOCUS III were positive
lines. For LOCUS III classification, the nucleus color affected OSI most
significantly, and posterior lens capsular also had secondly significant impact
on OSI. These results are similar to previous report[22]
and suggest the suitability of using the OSI as a tool for detecting incipient
cataracts.
We measured the OSI values at one day,
one week, two weeks, one month, and two months after surgery. With the
time increase, the OSI values were decreased until one month after surgery
which indicated that the eye conditions were stable from one month after
operation.
Our results showed that OSI values decreased both in
the spherical IOL and aspherical IOL groups compared with preoperative values.
Due to the opacity of the lens, the intraocular scattering of the preoperative
value was higher than that in a pseudophakic eye. In our study, the mean
preoperative OSI value was 12.0±3.6. The values calculated in our study were slightly
higher than those in previous studies[19,22].
The reason for the difference is that the degree of cataract in our study was
more serious than that in previous studies[19,22]. The OSI in the aspherical IOL implantation group was
lower than that in the spherical IOL implantation group. The reason for this
may be that the spherical aberrant reduction in the aspherical IOL implantation
group reduces the out-of-focus light, thus reducing the OSI value[23]. These results illustrate that reducing IOL aberration
improves visual quality.
In conclusion,
the OSI values measured by OQAS correctly isolates the information related to
intraocular scattering and highlights the relevance of pre and postoperative
optical quality evaluation in cataract patients. Our results showed that the
OSI values in the aspheric IOL group was lower than that in the spherical IOL
group, which indicates that the optical quality in the aspheric IOL group was
better than that in the spherical IOL group as measured by the OQAS.
ACKNOWLEDGEMENTS
Conflicts
of Interest: Chen Y, None; Wang X, None; Zhou CD, None; Wu Q,
None.
REFERENCES
1 Powe NR, Schein OD, Gieser SC, Tielsch JM, Luthra R, Javitt J,
Steinberg EP. Synthesis of the literature on visual acuity and complications
following cataract extraction with intraocular lens implantation. Arch Ophthalmol 1994;112(2):239-252. [CrossRef]
2
Rajabi MT, Korouji S, Farjadnia M, Naderan M, Rajabi MB, Khosravi B, Tabatabaie
SM. Higher order aberration comparison between two aspherical intraocular
lenses: MC6125AS and Akreos advanced optics. Int J Ophthalmol 2015;8(3):565-568. [PMC free article]
[PubMed]
3
Jia LX, Li ZH. Clinical study of customized aspherical intraocular lens
implants. Int J Ophthalmol
2014;7(5):816-821. [PMC
free article] [PubMed]
4
Kretz FT, Tandogan T, Khoramnia R, Auffarth GU. High order aberration and
straylight evaluation after cataract surgery with implantation of an aspheric,
aberration correcting monofocal intraocular lens. Int J Ophthalmol 2015;8(4):736-741. [PMC free article]
[PubMed]
5
Tang Y, Song H, Chen J, Tang X. Comparison of pseudophakic retinal straylight
in spherical/aspherical and hydrophobic/hydrophilic intraocular lens. Int J Ophthalmol 2015;8(6):1146-1150. [PMC free article]
[PubMed]
6
Liu J, Zhao J, Ma L, Liu G, Wu D, Zhang J. Contrast sensitivity and spherical
aberration in eyes implanted with AcrySof IQ and AcrySof Natural intraocular
lens: the results of a meta-analysis. PLoS
One 2013;8(10):e77860. [CrossRef]
7
Schuster AK, Tesarz J, Vossmerbaeumer U. The impact on vision of aspheric to
spherical monofocal intraocular lenses in cataract surgery: a systematic review
with meta-analysis. Ophthalmology
2013;120(11):2166-2175. [CrossRef]
8
Trueb PR, Albach C, Montés-Micó R, Ferrer-Blasco T. Visual acuity and contrast
sensitivity in eyes implanted with aspheric and spherical intraocular lenses. Ophthalmology 2009;116(5):890-895. [CrossRef]
9
Semeraro F, Romano MR, Duse S, Costagliola C. Quality of vision in patients
implanted with aspherical and spherical intraocular lens: Intraindividual
comparison. Indian J Ophthalmol
2014;62(4):461-463. [CrossRef]
10
Tzelikis PF, Akaishi L, Trindade FC, Boteon JE. Spherical aberration and
contrast sensitivity in eyes implanted with aspheric and spherical intraocular
lenses: a comparative study. Am J
Ophthalmol 2008;145(5):827-833. [CrossRef]
11 van Gaalen KW, Koopmans SA, Jansonius NM, Kooijman
AC. Clinical comparison of the optical performance of aspheric and spherical
intraocular lenses. J Cataract Refract
Surg 2010;36(1):34-43. [CrossRef]
12 Ye C, Ng PK, Jhanji V. Optical quality assessment
in normal and forme fruste keratoconus eyes with a double-pass system: a
comparison and variability study. Br J
Ophthalmol 2014;98(11):1478-1483. [CrossRef]
13 Hu AL, Qiao LY, Zhang Y, Cai XG, Li L, Wan XH.
Reproducibility of optical quality parameters measured at objective and
subjective best focuses in a double-pass system. Int J Ophthalmol 2015;8(5):1043-1050. [PMC free article] [PubMed]
14 Kamiya K, Shimizu K, Igarashi A, Kobashi H.
Effect of femtosecond laser setting on visual performance after small-incision
lenticule extraction for myopia. Br J Ophthalmol
2015;99(10):1381-1387. [CrossRef]
15 Xiao XW, Hao J, Zhang H, Tian F. Optical quality
of toric intraocular lens implantation in cataract surgery. Int J Ophthalmol 2015;8(1):66-71. [PMC free article] [PubMed]
16 Xu CC, Xue T, Wang QM, Zhou YN, Huang JH, Yu AY.
Repeatability and reproducibility of a double-pass optical quality analysis
device. PLoS One 2015;10(2):e0117587.
[CrossRef]
17 Martínez-Roda JA, Vilaseca M, Ondategui JC,
Aguirre M, Pujol J. Effects of aging on optical quality and visual function. Clin Exp Optom 2016;99(6):518-525. [CrossRef]
18 Kamiya K, Shimizu K, Igarashi A, Kobashi H. Time
course of optical quality and intraocular scattering after refractive lenticule
extraction. PLoS One 2013;8(10):e76738.
[CrossRef]
19 Artal P, Benito A, Perez GM, Alcon E, De Casas A,
Pujol J, Marín JM. An objective scatter index based on double-pass retinal
images of a point source to classify cataracts. PLoS One 2011;6(2):e16823. [CrossRef]
20 Santamaria J, Artal P, Bescós J. Determination of
the point-spread function of human eyes using a hybrid optical-digital method. J Opt Soc Am A 1987;4(6):1109-1114. [CrossRef]
21 Kamiya K, Shimizu K, Igarashi A, Kobashi H, Ishii
R, Sato N. Clinical evaluation of optical quality and intraocular scattering after
posterior chamber phakic intraocular lens implantation. Invest Ophthalmol Vis Sci 2012;53(6):3161-3166. [CrossRef]
22 Vilaseca M, Romero MJ, Arjona M, Luque SO,
Ondategui JC, Salvador A, Güell JL, Artal P, Pujol J. Grading nuclear, cortical
and posterior subcapsular cataracts using an objective scatter index measured
with a double-pass system. Br J
Ophthalmol 2012;96(9):1204-1210. [CrossRef]
23 Ohtani S, Gekka S, Honbou M, Kataoka
Y, Minami K, Miyata K, Oshika T. One-year prospective intrapatient comparison
of aspherical and spherical intraocular lenses in patients with bilateral
cataract. Am J Ophthalmol
2009;147(147):984-989. [CrossRef]