
·Letter to the Editor·Current Issue·
·Achieve·
·Search Articles· ·Online Submission· ·About IJO· PMC
Hallermann-Streiff syndrome with bilateral
microphthalmia, pupillary membranes and cataract absorption
Chun-Li Chen1, Jie Peng2,
Xin-Guo Jia1, Zheng-Wei Liu2, Pei-Quan Zhao2
1Department of Ophthalmology, Shengli Oilfield Central Hospital,
Dongying 257000, Shandong Province, China
2Department of Ophthalmology, Xin Hua Hospital Affiliated to
Shanghai Jiao Tong University School of Medicine, Shanghai 200092, China
Co-first
authors: Chun-Li Chen and Jie Peng
Correspondence to: Pei-Quan Zhao.
Department of Ophthalmology, Xin Hua Hospital Affiliated to Shanghai Jiao Tong
University School of Medicine, Shanghai 200092, China. zhaopeiquan@126.com
Received:
2016-10-18
Accepted: 2017-02-16
DOI:10.18240/ijo.2017.06.30
Citation: Chen CL, Peng J, Jia XG, Liu ZW, Zhao PQ.
Hallermann-Streiff syndrome with bilateral microphthalmia, pupillary membranes
and cataract absorption. Int J Ophthalmol 2017;10(6):1016-1018
Dear
Editor,
We
write to present a case report of Hallermann-Streiff syndrome (HSS;
oculo-mandibulo-dyscephaly with hypotrichosis) with persistent pupillary
membranes and cataract absorption.
CASE
REPORT
All
data and photos were taken with oral and written consent from the guardians.
The patient is a five-year old girl. She was a full-term baby with a normal
vaginal delivery with a birth weight of 2735 g and birth height of 50 cm. She
was the only baby in the family with no notable family history. Her mother’s
obstetric history revealed no record of systemic disease or drug
administrations. Her mother noticed that her daughter had a poor vision five
years ago. They visited local ophthalmic clinics two years ago and she was
diagnosed as having congenital cataract. No medical intervention was given. Recently,
they resorted to us showing typical dyscephalia of the HSS (bird face) (Figure
1A, 1B).

Figure
1 The typical “bird-face” with mandibular hypoplasia A: Frontal
view; B: Profile view; C: Esotropia.
The
patient was once diagnosed as proportionate short suture and growth retardation
at three-year old. She has received growth hormone injection therapy for a year
already. On admission to our facility, she was five years and four months old,
and her height was 94 cm while the body weight was 12 kg. The head
circumference was 48 cm and normal. Four limbs were thin with normal muscle
forces. She had a pointed nose and frontal bossing (Figure 1A, 1B). Her hairs
were thin and brows absent. Her skin was so thin that the vessels were
prominent. All nails were normal. She had a small mandible and irregular
cone-shape teeth. Her ears were small and close to the mastoid process without
listening problems. The patient had no cardiac or respiratory disorders, or
mental retardation.
Entropion
and trichiasis were observed on the upper lids. Epiblepharon of the upper
palpebra were observed. Palpebral fissure was 24 mm in width and 8 mm in
height. Bilateral inner canthus distance was 28 mm. Both eyes showed
microphthalmia and microcornea [cornea diameter of right eye
vertical/horizontal (V/H)=8.5/8.3 mm, left eye (V/H)= 8.5/8.3 mm]. Involuntary
horizontal nystagmus of both eyes as well asesotropia of near 30 prism diopter
(PD) (Figure 1C) was noted. Vision acuity of both eyes was finger counting at 1
m. The intraocular pressures were normal.
Corneas
and anterior chambers were clear. Pupillary membrane and miosis due to
posterior synechiae were observed, making fundus examination impossible (Figure
2A). The pupil diameter was 1.8 mm of the left eye and 1.6 mm of the right eye.
Depths of anterior chamber of both eyes were 24 mm. The opaque lenses were
thin. Ultrasound test revealed mild vitreous opacity in the left eye and no
retinal detachment in both eyes. No clear echoic reflection of posterior lens capsule
was detected indicating lens absorption. A-scan showed short optic axis
lengths, 16.45 mm for the right eye and 15.54 mm for the left eye. However, due
to binocular nystagmus, errors do exist. The electroretinogram showed decreased
amplitudes of a-wave and b-wave after both dark and light adaptation. And
flash-vision evoked potential of both eyes was normal.
SURGICAL
TREATMENT
Resection
of the pupillary membranes and lensectomy were performed in both eyes under
general anesthesia without problem in securing endotracheal intubation. During
the surgery, lens absorption and thin lens covered with double-folded membrane
was verified (Figure 2B, 2C). These thick membranes presumably were remnants of
the anterior and posterior capsules. Intraocular lens implantation was not
performed due to microphthalmia.
The
first day after the surgery, the pupils were round, regular and equal (Figure
2D). The optic axis was clear and fundus was normal. However, examinations of
the periphery or fundoscopy were not possible due to nystagmus and poor
cooperation. Eyeglasses and amblyopia training were prescribed. The best
corrected vision acuity of both eyes one week after the surgery were 0.02 (OD:
+16.00DS/-2.50DC×170°; OS: +17.50DS/-2.75DC×20°) by Chinese Standard
Logarithmic Visual Acuity Chart. The intraocular pressure was normal.
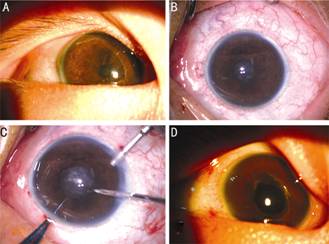
Figure
2 Images of the right eye A: Before
the surgery, pupillary membrane and miosis were observed; B: After pupil
dilation, miosis remained due to posterior synechiae; C: The lens was absorbed
and replaced by opaque membranes; D: The first day after the surgery, the pupil
was round and no uveitic reaction was noted.
DISCUSSION
HSS
is a rare disease. It is characterized by bird-like face, dental abnormalities,
hypotrichosis, atrophy of skin, proportionate nanism, congenital cataracts and
bilateral microphthalmia[1]. HSS was initially noted in 1983,
however the description was not complete. This syndrome was first described by
Hallermann in 1948 and by Streiff in 1950. In 1953, it was first identified as
an independent syndrome. Well-accepted diagnostic criteria was established by
Francois[2] in 1958. Virtually all cases are sporadic. There is no
sex predilection[1].
Over
150 cases of HSS have been reported worldwide since it was first described as
HSS by Francois[2-3] in 1958. The diagnostic criteria of this entity
include dyscephalia and bird face (98%-99%), dental anomalies (80%-85%),
proportionate nanism (45%-68%), hypotrichosis (80%-82%), atropy of the skin
(68%-70%), bilateral microphthalmia (78%-83%) and congenital cataract (81%-90%)[1-2].
This patient had all seven features.
Ocular
anomolies are a major problem, with the most common changes being
microphthalmia and cataracts, presenting in 81%-90% of HSS patients[1,3].
The lenses may have been absorbed spontaneously after birth, which sometimes
occurs in the setting of HSS[3-6]. Other ocular finding of HSS
include microphthalmia (78%-83%), nystagmus (32%-45%), strabismus (33%-37%),
blue sclera (22%-31%), sparse eyelashs and eyebrows (29%), fundus anomalies
(18%-22%), conjunctival defects (11%), cornea abnormalities (9%-14%),
down-slanting palpebral fissures (12%-13%) and so on[1].
In
this case, entropion and trichiasis, epiblepharon, nystagmus, esotropia, absence
of brows, microphthalmia, microcornea, pupillary membrane, miosis, posterior
synechiae and bilateral lens absorption were found. The diagnosis is easily
made. Bilateral microphthalmia and congenital cataract are often manifested[7].
Cataract absorption is the result of untreated congenital cataract. The
pupillary membrane could be the result fibrinous reaction after cataract
rupture and absorption.
For
this case, poor vision was found in the first year of life. However, the
treatment was delayed until the patient was five-year old, making vision
rehabilitation more difficult. This makes it urgent for early ocular screening
and treatment for HHS patients.
Besides,
one of the most severe complications in HSS is respiratory embarrassment[1].
Fortunately, this patient had no problem in tracheal intubation during the
anesthesia and recovered from anesthesia without any respiratory complications.
Close follow-up is needed.
CONCLUSION
In
conclusion, we present a case of successful surgical repair for HSS in a
five-year old patient who had ophthalmic features of pupillary membranes,
posterior synechiae and lens absorption. In the setting of HSS, ocular
examinations should be performed immediately when the patient was diagnosed.
Cataract should be removed as early as possible to restore the vision
functions.
ACKNOWLEDGEMENTS
Foundations: Supported
by the National Natural Science Foundation of China (No.81271045; No.81470642);
Shanghai Science and Technology Committee (No.15XD1502800).
Conflicts
of Interest: Chen CL, None; Peng J, None; Jia XG,
None; Liu ZW, None; Zhao PQ, None.
REFERENCES
1 Cohen MM Jr.
Hallermann-Streiff syndrome: a review. <ii>Am J Med Genet
</ii>1991;41(4):488-499. [CrossRef] [PubMed]
2 Francois J. A new
syndrome; dyscephalia with bird face and dental anomalies, nanism,
hypotrichosis, cutaneous atrophy, microphthalmia, and congenital
cataract.<ii> AMA Arch Ophthalmol </ii>1958;60(5):842-862. [CrossRef]
3 David LR, Finlon M,
Genecov D, Argenta LC. Hallermann-Streiff syndrome: experience with 15 patients
and review of the literature. <ii>J Craniofac Surg </ii>1999;10(2):160-168.
[CrossRef]
4 Park HJ, Lee SJ,
Kim WS. A case of Hallermann-Streiff syndrome.<ii> J Korean Ophthalmol
Soc </ii>2007;48(9):3356-3357. [CrossRef]
5 Ryoo MH, Kim SS, Yi
KP. A case of Hellermann-Streiff syndrome. <ii>J Korean Ophthalmol Soc
</ii>1990;31(6):831-836.
6 Soriano JM, Funk J.
Spontaneous bilateral lens resorption in a case of Hallermann-Streiff syndrome.
<ii>Klin Monbl Augenheilkd </ii>1991;199(3): 195-198. [CrossRef] [PubMed]
7 Myung Chul Lee, Im
Jeong Choi, Jin Wha Jung. A case of Hallermann-Streiff syndrome with
aphakia.<ii> Korean J Pediatr </ii>2008;5(6)1:646-649.