INTRODUCTION
Keratoconus is a bilateral, non-inflammatory ectatic disease characterized by central corneal thinning, corneal apical protrusion, and irregular astigmatism[1-2]. Classic features of the disease include focal scarring, breaks in Bowman’s layer,and iron deposits in the epithelial basement membrane[2-3].Patients may also develop photophobia, glare, and monocular diplopia[4]. As the disease progresses, myopia increases and image quality is further reduced by higher-order ocular aberrations[5]. Eventually, myopia and irregular astigmatism lead to a decrease in visual acuity[6-7]. In advanced disease,axial corneal scarring can develop, leading to further impairment of vision[2]. The exact etiology and pathogenesis of keratoconus are not known; however, various genetic and environmental risk factors have been implicated[1-2,8].
The main aims of the keratoconus treatment are to stop the progression of ectasia, improve refractive error and aberrations, and restore the normal shape of the cornea[9].The management of keratoconus varies with disease severity.Historically, mild keratoconus has been managed with eyeglasses while moderate keratoconus has been treated with contact lenses. Until recently, the only treatment option for keratoconus in patients intolerant to contact lenses was corneal transplantation. Although penetrating keratoplasty is one of the most common types of corneal transplant, this procedure can be complicated by recurrent disease, serious side effects, and a lengthy recovery time.
When excimer laser refractive surgery was first introduced,it was touted as a procedure that could reduce the need for keratoplasty in keratoconus patients. Unfortunately, reports of increased risk of keratectasia after laser-assisted in situ keratomileusis (LASIK) and photorefractive keratectomy(PRK) caused many surgeons to consider excimer laser treatment as a contraindication for keratoconus for more than a decade. Advances in laser technology and approval of corneal collagen cross-linking (CXL) have allowed practitioners to rethink this position[9]. Today, PRK is again considered as an alternative to keratoplasty when used with CXL[10]. CXL uses UVA to activate riboflavin and create covalent bonds between collagen fibrils, resulting in increased biomechanical strength of the cornea[11-12]. The goals of simultaneous treatment with PRK/CXL combination treatment are to strengthen the cornea and stop disease progression with CXL and improve vision through laser ablation.
The aim of this study was to report the long-term visual outcomes of patients who had undergone combined nontopography-guided PRK and CXL (non-TG-PRK+CXL) for the treatment of keratoconus.
SUBJECTS AND METHODS
The present case series gathered information in a prospective manner. The included patients had undergone combined non-TG-PRK+CXL between January 2008 and December 2016 at Magrabi Aseer Eye Hospital, Khamis Mushait, Saudi Arabia.The Institutional Review Board of King Khalid University in Abha, Saudi Arabia approved the study protocol. Written informed consent was obtained from all patients. This study adhered to the tenets of the Declaration of Helsinki.
Inclusion and Exclusion Criteria Patients between the age of 21 and 41y with keratoconus (stage 1 or 2), which had not progressed for a year before the study, and had undergone combined non-TG-PRK+CXL were included in the study.Other inclusion criteria are as follows: intolerant to contact lens, had a corneal thickness of >400 μm at the thinnest point,and had no other corneal pathological signs.
Pregnant and lactating women, patients with corneal scarring,previous intraocular surgery, incomplete documentation,insufficient postoperative care or follow-up, concomitant eye disease, autoimmune disease, or with a history of herpetic keratitis were excluded from the study.
Outcome Measures The primary outcome measures for our study were changes in visual acuity and refraction. All adverse events that occurred during the study period were monitored and documented. All measures were recorded preoperatively and postoperatively at all follow-up visits.
Methodology Patients planned to be included in the study had previously undergone combined non-TG-PRK+CXL(Quest excimer laser platform, NIDEK Co. Ltd., Japan) with conventional ablation profile. The analysis was restricted to the records of patients with topography pattern consistent with keratoconus and an inferior-superior ratio >1.5 on topography mapping and a preoperative corrected distance visual acuity(CDVA) ≥0.3 (logMAR). All had stage 1 or 2 keratoconus as defined based on the Amsler-Krumeich classification (i.e.,minimum corneal thickness >400 μm, mean keratometry readings<53.00 D with myopia and/or astigmatism not more than 8.00 D, and no corneal scarring)[13-15].
Clinical Evaluation
Pre- and postoperative ophthalmologic evaluation Standard demographic information, medical and family history were collected from each patient chart. Preoperative evaluation consisted of complete ophthalmic examinations, including autorefractometry and autokeratometry (Nidek Autorefractor Keratometer, Middlesex, UK), corneal topography (OCULUSPentacam®, Optikgeräte GmbH, Wetzlar, Germany), and slitlamp examination of the anterior and posterior segments of the eye. Pre- and postoperative uncorrected distance visual acuity(UDVA) and CDVA, keratometry, and manifest refraction were measured before surgery and at each postoperative visit.All patients were followed postoperatively. The first followup visit was at 5d, after which patients were seen at 3mo and yearly for 5y.
Surgical procedures All procedures were performed by the same surgeon (Al-Amri AM). After topical anesthesia with benoxinate HCl, Benox®0.4% eye drop (Benox®, Eipico, Egypt)was applied, and the epithelium was removed mechanically using a Beaver surgical blade (8.00 mm in diameter). PRK was performed with Quest excimer laser platform (NIDEK Co.Ltd., USA). Mitomycin 0.2 mg/mL was then applied for 10s,and PRK was immediately followed by CXL.
Hypotonic riboflavin solution (0.1% topical riboflavin sodium phosphate) was added and then ultrasonic pachymetry(Sonogage Corneo-Gage Plus, USA) was performed. If the cornea was <400 μm, additional hypotonic riboflavin solution was administered for 30min until the stroma had swollen to at least 400 μm. The cornea was then exposed to UVA (UVX 1000; IROC, Zurich, Switzerland) 365 nm light for 15min at an irradiance of 3.0 mW/cm2. During UVA exposure,hypotonic riboflavin solution (0.1% one drop every 2min) was continued every 2min.
Postoperatively, topical antibiotic (moxifloxacin) and corticosteroid (fluorometholone) drops (6 hourly and steroid tapered over 6wk) were administered and continued for 1wk and 6wk, respectively. A therapeutic soft contact lens (Acuvue,USA) (soft contact lens was used in all patients) was placed.The contact lens was removed after epithelial healing. Patients were followed for 3mo postoperatively and had complete examinations yearly for 5y.
Statistical Analysis Statistical analysis was performed using SPSS version 22 (SPSS Inc., Chicago, IL, USA). P<0.05 was considered statistically significant.
RESULTS
Study Patients A total of 30 patients between the age of 21 and 41y of age (28.5±5.4y) were included in the study, and almost half of the study population was male (n=16, 53.3%)(Figure 1). All patients had keratoconus in both eyes. The mean duration of follow-up was 68.20±4.71mo (range: 60-106mo),which was done at 3mo and yearly for 5y postoperatively(Table 1). However, the results were collated by comparing clinical parameters at preoperative visit with last follow-up visit (5y).
Visual Outcome All patients showed a significant (P<0.05)improvement in visual acuity and refraction after surgery at 5-year follow-up visit. Patients showed a significant improvement (P<0.05) in UDVA from 1.24±0.79 logMAR(range 0.7 to 1.7) prior to combined non-TG-PRK+CXL to 0.06±0.15 logMAR (range 0.04 to 0.7) at the time of their last follow-up visit (Figure 2). Seventy-eight percent of patients improved by 2 or more lines of uncorrected distance visual acuity postoperatively. CDVA significantly increased from 0.06±0.19 logMAR preoperatively (range 0.05 to 0.7)to 0.03±0.12 logMAR postoperatively (range 0.04 to 0.6)(P<0.05) (Figure 3). Eighty-one percent of eyes improved by 2 or more lines of CDVA postoperatively. In terms of safety, no eye lost lines of CDVA.
Refractive Outcome A significant decrease in the mean spherical equivalent (SE) refraction was observed from-2.28±1.8 (range 1.75 to 4.75) to -0.79±0.93 diopters (D)(range 1.75 to 0.75) (P<0.05), and the mean manifest cylinder decreased from -1.73±0.86 preoperatively (range -5.5 to 0)to -0.29±0.34 postoperatively (range 0.50 to 0) (P=0.001)(Figures 4, 5).
Topographic Outcome The mean keratometric values(Ksteep) were significantly reduced at 5-year follow-up visit, from 47.28±2.12 preoperatively to 45.13±1.32 D postoperatively(P<0.05) (range 44.9 to 49.7).
The preoperative mean steepest keratometry (Kmax) 48.6 (SD 3.1, range 47.4 to 52.9) was reduced significantly to 46.8 D(SD 2.9, range 46.2 to 53.4) postoperatively (P<0.05).
The preoperative mean flat keratometry (Kflat) 43.82±2.8(range 42.7 to 46.8) was reduced significantly to 41.6±1.89(range 40.2 to 44.1) postoperatively (P<0.05) (Figures 6, 7).
No evidence of Kmax progression over the follow up period(P>0.05).
Preoperative mean keratometric astigmatism was reduced from-3.21±1.47 D (SD 2.87, range 2.72 to 4.38) preoperatively to -1.65±0.69 postoperatively (SD 2.18, range 1.5 to 2.75)(P=0.05).
Adverse Events There were no serious intraoperative or postoperative complications or adverse events (AEs) reported in any of the patients. Two patients (4 eyes) developed mild corneal haze. None of the subjects developed infectious keratitis. Only three patients (6 eyes) experienced dry eyes.

Figure 1 Gender distribution.
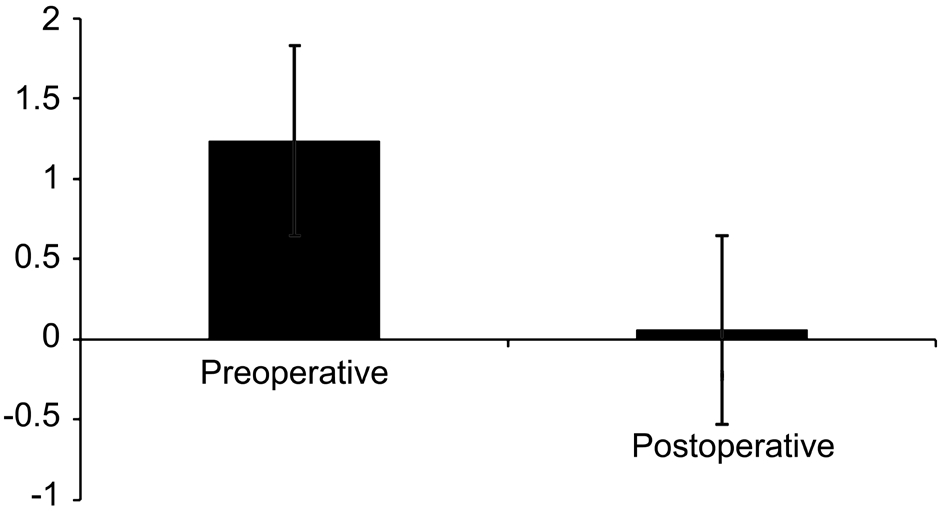
Figure 2 UDVA (logMAR) mean values.
Table 1 Pre- and postoperative follow-up data mean±SD
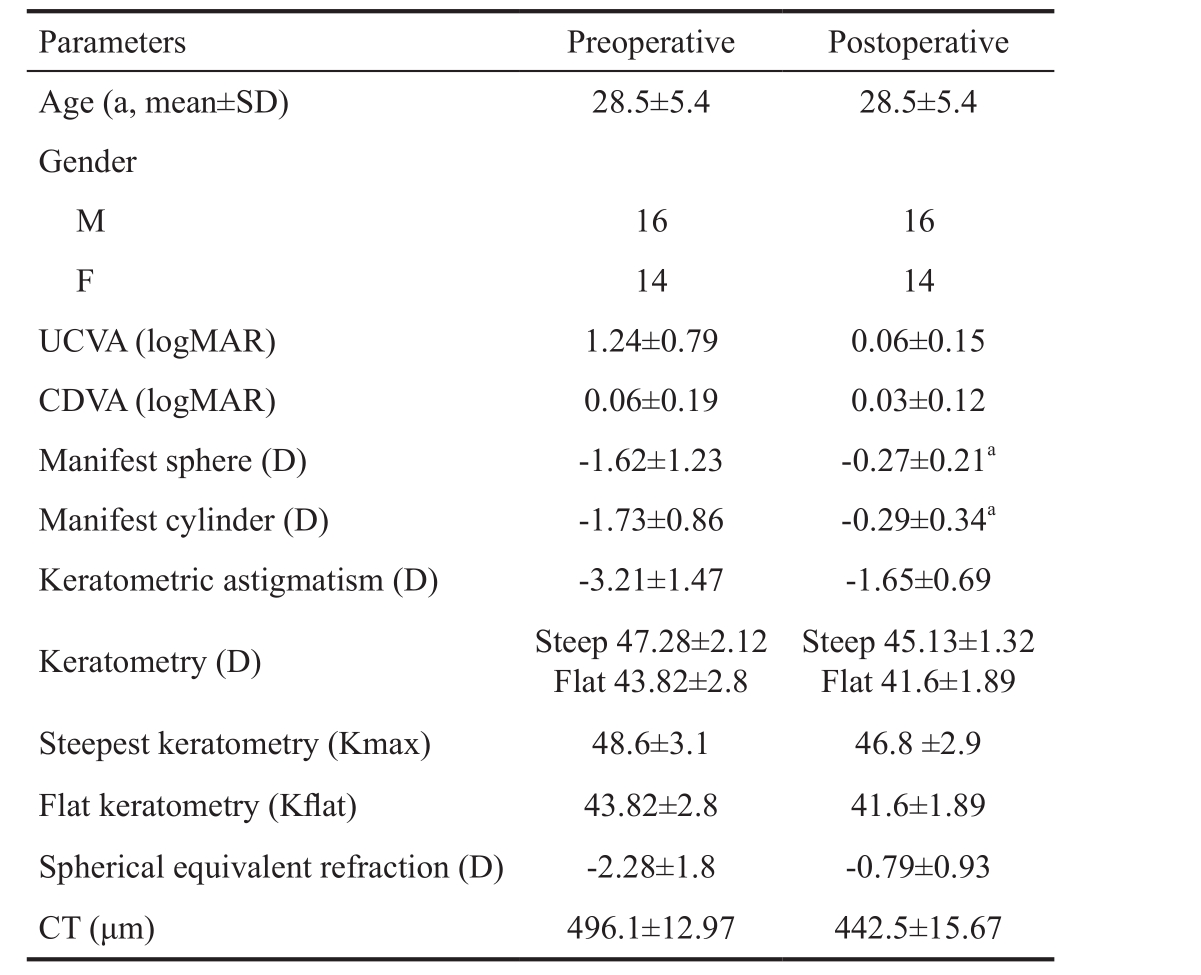
UCVA: Uncorrected visual acuity; CDVA: Corrected distance visual acuity; CT: Corneal thickness.aP<0.05, n=30 patients (60 eyes).
DISCUSSION
Conventionally, keratoconus has always been considered a contraindication for PRK; however, clinical studies have shown that CXL alone is also not an effective treatment for keratoconus. Hence, for better results, CXL should be combined with other surgical options as well[16-21]. This trend has highlighted the possibility of combining CXL and PRK as a treatment option for patient with stable keratoconus[16].The two most commonly used PRK+CXL techniques are TGPRK+CXL and non-TG-PRK+CXL.

Figure 3 CDVA (logMAR) mean values.
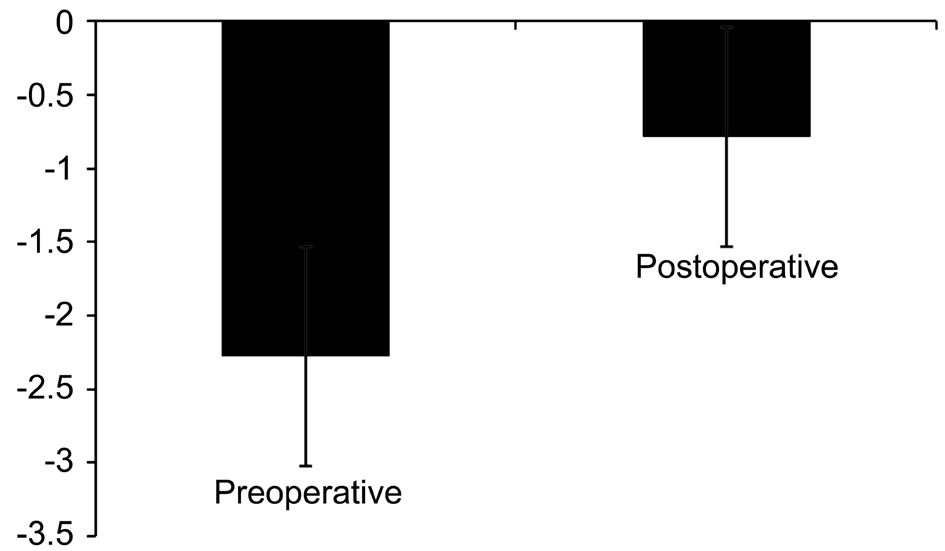
Figure 4 SE refraction (D) mean values.

Figure 5 Manifest cylinder (D) mean values.
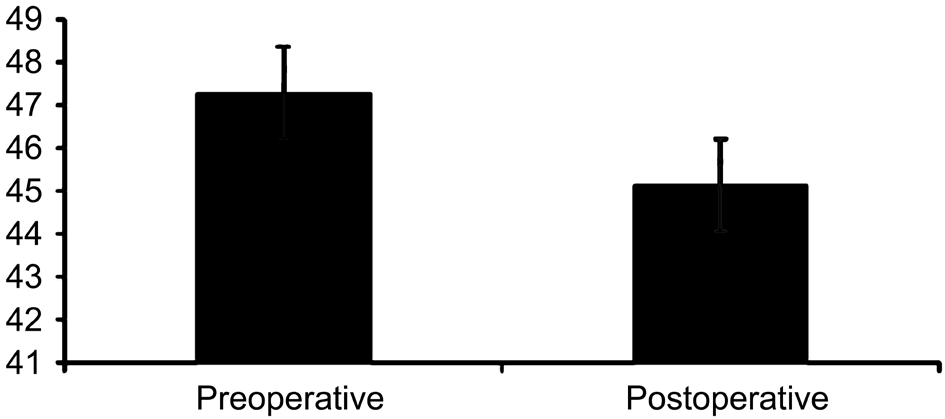
Figure 6 Keratometry (D) steep mean values.
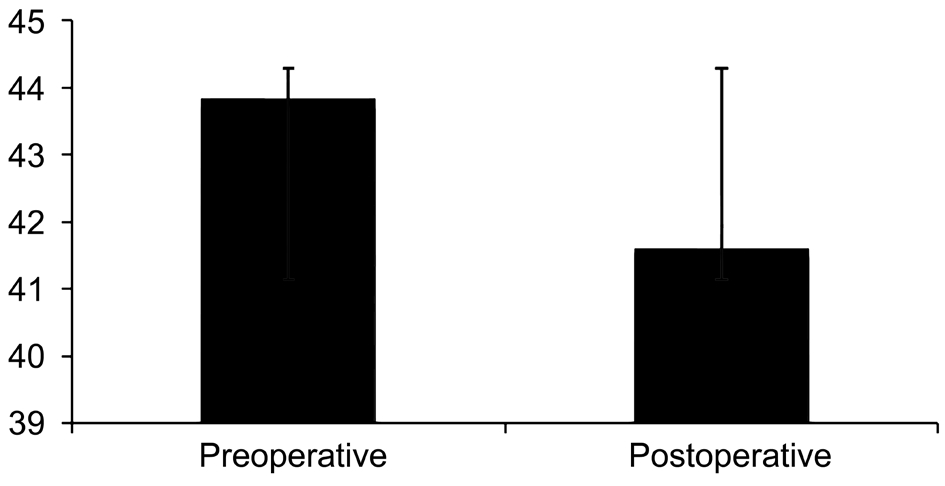
Figure 7 Keratometry (D) flat mean values.
Although studies have demonstrated the efficacy and safety of TG-PRK plus CXL for patients with mild to moderate keratoconus, yet the lack of data regarding the long-term stability of TG-PRK plus CXL remained the major limitation of this procedure[4,9].
Currently, only two studies have evaluated the efficacy of non-TG-PRK+CXL in correcting refractive errors in patients with keratoconus[17,21]. The findings of these studies suggest that for patients with mild-to-moderate keratoconus, non-TGPRK+CXL is safe and effective. Fadlallah et al[17]reported that non-TG-PRK after intracorneal ring segment (ICRS)implantation and CXL was found to be an effective and safe option for correcting residual refractive error and improving visual acuity in patients with moderate keratoconus[21],Additionally Fadlallah et al[17]evaluated the safety and clinical outcome of combined non-TG-PRK and CXL for the treatment of mild refractive errors in patients with early stage keratoconus and reported that combined non-TG-PRK and 30min CXL is an effective and safe option for patients with early stable keratoconus[17]. Also, in the present study, all patients were followed postoperatively with the first followup visit at 5d, followed by which the patients were seen at 3mo and yearly for 5y. Such prolonged follow-up of patients helped provide important information on both efficacy and safety outcomes. Our study evaluated the efficacy of non-TGPRK combined with 15min CXL in mild-to-moderate stage of keratoconus with no hyperopic shift and no haze.
The CDVA (0.03±0.12) was found to be similar in both studies,but the UDVA (0.06±0.19) was better in the current paper. The keratometry (flat/steep) and SE were also found to be better with the techniques used in the current paper. However, the small sample size (30 patients, 60 eyes) and single center study are the major limitations of our study.
In conclusion, combined non-TG-PRK+CXL demonstrate good 5-year outcomes in patients with mild, stable keratoconus.Therefore, we recommend conducting future large scale,comparative, randomized trials with extended duration of follow up to establish the long-term stability of this procedure in keratoconus. Findings from such studies could prove helpful in having generalized clinical guidelines and strategies for the management of keratoconus
ACKNOWLEDGEMENTS
Conflicts of Interest: Al-Amri AM, None.
REFERENCES
1 Rabinowitz YS. Keratoconus. Surv Ophthalmol 1998;42(4):297-319.
2 Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol 1984;28(4):293-322.
3 Andreassen TT, Simonsen AH, Oxlund H. Biomechanical properties of keratoconus and normal corneas. Exp Eye Res 1980;31(4):435-441.
4 Kanellopoulos AJ, Asimellis G. Revisiting keratoconus diagnosis and progression classification based on evaluation of corneal asymmetry indices, derived from Scheimpflug imaging in keratoconic and suspect cases. Clin Ophthalmol 2013;7:1539-1548.
5 Miháltz K, Kovács I, Kránitz K, Erdei G, Németh J, Nagy ZZ.Mechanism of aberration balance and the effect on retinal image quality in keratoconus: optical and visual characteristics of keratoconus. J Cataract Refract Surg 2011;7(5):914-922.
6 Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet a cornealcollagen cross-linking for keratoconus in Italy: the Siena eye cross study. Am J Ophthalmol 2010;149(4):585-593.7 Vinciguerra P, Albè E, Trazza S, Seiler T, Epstein D. Intraoperative and postoperative effects of corneal collagen cross-linking on progressive keratoconus. Arch Ophthalmol 2009;127(10):1258-1265.
8 Spörl E, Huhle M, Kasper M, Seiler T. Increased rigidity of the cornea caused by intrastromal cross-linking. Ophthalmologe 1997;94(12):902-906.
9 Ormonde S. Refractive surgery for keratoconus. Clin Exp Optom 2013;96(2):173-182.
10 Kymionis GD, Kontadakis GA, Kounis GA, Portaliou DM, Karavitaki AE, Magarakis M, Yoo S, Pallikaris IG. Simultaneous topography-guided prk followed by corneal collagen cross-linking for keratoconus. J Refract Surg 2009;25(9):S807-S811.
11 Wollensak G. Crosslinking treatment of progressive keratoconus: new hope. Curr Opin Ophthalmol 2006;17(4):356-360.
12 Dahl BJ, Spotts E, Truong JQ. Corneal collagen cross-linking: an introduction and literature review. Optometry 2012;83(1):33-42.
13 Kamiya K, Ishii R, Shimizu K, Igarashi A. Evaluation of corneal elevation, pachymetry and keratometry in keratoconic eyes with respect to the stage of Amsler-Krumeich classification. Br J Ophthalmol 2014;98(4):459-463.
14 Ishii R, Kamiya K, Igarashi A, Shimizu K, Utsumi Y, Kumanomido T. Correlation of corneal elevation with severity of keratoconus by means of anterior and posterior topographic analysis. Cornea 2012;31(3):253-258.
15 Toprak I, Yaylali V, Yildirim C. A combination of topographic and pachymetric parameters in keratoconus diagnosis. Cont Lens Anterior Eye 2015;38(5):357-362.
16 Mastropasqua L. Collagen cross-linking: when and how? A review of the state of the art of the technique and new perspectives. Eye Vis (Lond)2015;2:19.
17 Fadlallah A, Dirani A, Chelala E, Antonios R, Cherfan G, Jarade E.Non-topography-guided PRK combined with CXL for the correction of refractive errors in patients with early stage keratoconus. J Refract Surg 2014;30(10):688-693.
18 Goldich Y, Marcovich AL, Barkana Y, Avni I, Zadok D. Safety of corneal collagen cross-linking with UV-A and riboflavin in progressive keratoconus. Cornea 2010;29(4):409-411.
19 Vinciguerra P, Albè E, Trazza S, Rosetta P, Vinciguerra R, Seiler T, Epstein D. Refractive, topographic, tomographic, and aberrometric analysis of keratoconic eyes undergoing corneal cross-linking. Ophthalmology 2009;116(3):369-378.
20 Kymionis GD, Portaliou DM, Kounis GA, Limnopoulou AN,Kontadakis GA, Grentzelos MA. Simultaneous topography-guided photorefractive keratectomy followed by corneal collagen cross-linking for keratoconus. Am J Ophthalmol 2011;152(5):748-755.
21 Guedj M, Saad A, Audureau E, Gatinel D. Photorefractive keratectomy in patients with suspected keratoconus: five-year follow-up. J Cataract Refract Surg 2013;39(1):66-73.