·Meta-Analysis·
Effcacy and safety of vitrectomy with internal limiting membrane peeling for diabetic macular edema: a Metaanalysis
Xin-Ying Hu1, Huan Liu1, Li-Na Wang2, Yu-Zhi Ding1, Jie Luan1
1Department of Ophthalmology, Zhongda Hospital, Southeast University, Nanjing 210009, Jiangsu Province, China
2Department of Epidemiology & Biostatistics, School of Public Health, Southeast University, Nanjing 210009, Jiangsu Province, China
Abstract
● AlM:To evaluate the efficacy and safety of vitrectomy with internal limiting membrane (lLM) peeling for diabetic macular edema (DME).
● METHODS:The PubMed, Embase, Web of Science,Cochrane, SionMed, ClinicalTrials.gov, CNKl databases and Wanfang databases, published until Oct.2017, were searched to identify studies comparing the clinical outcomes following vitrectomy with and without lLM peeling, for treating DME.Pooled results were expressed as odds ratios (ORs) with corresponding 95% confdence intervals (Cl) for vitrectomy with and without lLM peeling with regard to best corrected visual acuity (BCVA), central macular thickness (CMT), and complication incidents.
● RESULTS:A total of 14 studies involving 857 eyes were included of which three studies were Chinese and the rests were English literatures.Meta-analysis indicated that compared with vitrectomy alone, vitrectomy with lLM peeling could improve BCVA more obviously (OR=1.66,95%Cl: 1.12-2.46,P=0.01) and had higher rate of CMT reduction (OR=3.89, 95%Cl: 1.37-11.11,P=0.01).There were signifcant statistical differences between the two surgical methods for both BCVA and CMT (P<0.05).For the incidence of intraoperative and postoperative complications, the incidence of epiretinal membrane (ERM) was slightly lower in the lLM peeling group than the group without lLM peeling (OR=0.38, 95%Cl: 0.07-2.00,P=0.25), although insignifcant statistically.Other incidences of overall complications, iatrogenic peripheral retinal break and increased intraocular pressure indicated no significant difference between two groups (OR=1.19, 95%Cl: 0.82-1.73,P=0.36; OR=1.21, 95%Cl: 0.66-2.21,P=0.53; OR=1.34,95%Cl: 0.75-2.40,P=0.32).
● CONCLUSlON:Vitrectomy is effective for DME and the effect can be improved by additional lLM peeling,especially for anatomical effcacy, without increasing the incidence of intraoperative and postoperative complications.However, it is imperative to gain more evaluation in the future due to the paucity of prospective randomized study.
● KEYWORDS:internal limiting membrane; vitrectomy;diabetic macular edema; Meta-analysis
INTRODUCTION
Diabetic retinopathy is one of the major chronic complications of diabetes mellitus (DM) as well as a main reason of visual loss.Diabetic macular edema (DME) is an ocular manifestation of the disease that causes vision deterioration[1].It progressively decreases visual acuity (VA), with more than half of the patients losing at least 2 lines within 2y[2].In addition to controlling blood glucose, blood pressure, blood lipids and optimizing internal medicine therapy, anti-vascular endothelial growth factor (VEGF) drugs, steroids, laser photocoagulation and pars plana vitrectomy (PPV) are the main methods of DME treatment.The retinal internal limiting membrane (ILM) is a basement membrane that defines the boundary between the vitreous and the retina.It consists of the internal expansions of Müller cells and a meshwork of glycosaminoglycans, collagen fibers, laminin and fibronectin called the cuticular layer[3].Müller cells can migrate to the inner surface of the ILM and form a membranous contraction structure, resulting in the contractile force in tangential direction.As a basement membrane, ILM can serve as a framework for cell proliferation and is often involved in diseases that affect the vitreomacular interface[3-4].Recently, the signifcance of ILM peeling has been investigated in surgical management of DME.Several scholars stated a positive effect of ILM peeling during vitrectomy for DME.It has been hypothesized that ILM peeling has more favorable anatomical and visual results[5-6].However, some studies have reported minimal improvement of VA outcomes compared to baseline.The aim of this Meta-analysis is to explore the effectiveness and safety of ILM peeling adjunct to vitrectomy in DME surgery.
MATERIALS AND METHODS
Literature ReviewA literature review was executed to determine all relevant studies comparing the outcomes of vitrectomy with and without ILM peeling for DME.The PubMed, Embase, Web of Science, Cochrane, SionMed,ClinicalTrials.gov, Wanfang and China National Knowledge Infrastructure (CNKI) databases were searched for all articles systematically published before Oct.2017.We have no language restrictions.The following terms were applied for the search: (“internal limiting membrane” OR “inner limiting membrane” OR “ILM”) and (“macular edema” OR“diabetic retinopathy” OR “DME”).We manually searched the reference lists of all retrieved articles to expand our search.All articles are managed with Endnote X7.The study and data accumulation were carried out with approval from the Institutional Review Board of Southeast University Zhongda Hospital.
Take PubMed as an example: {[(macular edema) OR (diabetic retinopathy) OR DME] AND [(internal limiting membrane)OR (inner limiting membrane) OR ILM]}.
Data Extraction and Quality AssessmentTwo reviewers(Hu XY and Liu H) reviewed the title and abstracts of each study independently, and studies which satisfed the inclusion criteria were selected.For each study selected, we collected the data as follows: frst author, year of publication, country,sample size, average age, preoperative best-corrected visual acuity (BCVA), preoperative central macular thickness (CMT),outcomes, complications and follow-up time.Differences between the two reviewers were resolved through discussion or a third reviewer (Ding YZ).Because not all selected studies were randomized controlled trial (RCT), nonrandomized trials were assessed according to the Methodological Index for Nonrandomized Studies (MINORS) on a scale of 0 to 24[7]and RCTs were assessed as “low”, “high” or “unclear” risk of bias according to the Cochrane Collaboration Reviewers”Handbook[8].Nonrandomized trials with a score of ≥18 were considered to be of relatively high quality.Two independent reviewers (Hu XY and Liu H) assessed the quality and discrepancies were resolved through discussion.
Criteria for Inclusion and ExclusionThe inclusion criteria were as follows: 1) study design: clinical comparative studies that comparing the outcomes between patients receiving vitrectomy with ILM peeling and those without ILM peeling for DME; 2) study object: patients have been diagnosed with DME without age, sex, race limited; 3) intervention:studies included vitrectomy and included at least two groups(with and without ILM peeling); 4) follow-up time: studies with a minimum follow-up period of 3mo; 5) outcome evaluation index: the outcomes were evaluated with one or more comparisons as follows: rate of vision improvement, rate of CMT reduction, and complication incidence at the end of follow up.The exclusion criteria were as follows: 1) noncomparative studies, letters, abstracts, editorials, experts opinions and reviews lack of original data; 2) the results or relevant parameters of patients were not clearly stated and it was impossible to extract or calculate the data from the results published; 3) follow-up time of studies was less than 3-month; 4) only title related to ILM peeling while content was not mentioned; 5) articles repeated published or with duplicated contents.
Statistical AnalysisThe Meta-analysis was conducted using Review Manager (V.5.3, the Cochrane Collaboration,Oxford, England, UK) and Stata software (version 12.0;Stata Corp, College Station, Texas, USA).We evaluated the effect and safety of vitrectomy with ILM peeling or not by three outcomes: data of functional efficacy, as assessed by the rate of vision improvement; data of anatomical efficacy,as assessed by the rate of CMT reduction; data of safety, as assessed by the incidence of complications.We analyzed the proportion among BCVA improvement, CMT reduction, and complication incidents as classified variables and calculated the odds ratios (ORs) with 95% confidence intervals (CIs).ORs were generally considered statistically significant atP<0.05.Heterogeneity was evaluated by calculating theI2statistic as well as performing the Chi-square test (to assess thePvalue).TheI2statistic, refers to the proportion of total variation observed between the trials rather than the sampling error.Higginset al[9]reported that theI2ranges were from 0 to 100%, and whenI2=0, there was no heterogeneity in the study.A greaterI2value means, a higher chance of heterogeneity.AnI2value larger than 50%, indicated a moderate to high heterogeneity.When no heterogeneity was detected, a fixedeffects model was applied, which meant that there were no variances among all studies.If any heterogeneity detected,a random-effects model, which caused wider CIs than the fixed-effects model, was used for this study.For a high heterogeneity result, a Meta-regression which calculated by an average summary value was applied to determine the source of heterogeneity.Some possible moderators were tested to explore the heterogeneity.Egger’s regression and Begg’s test were applied to detect the presence of publication bias.
RESULTS
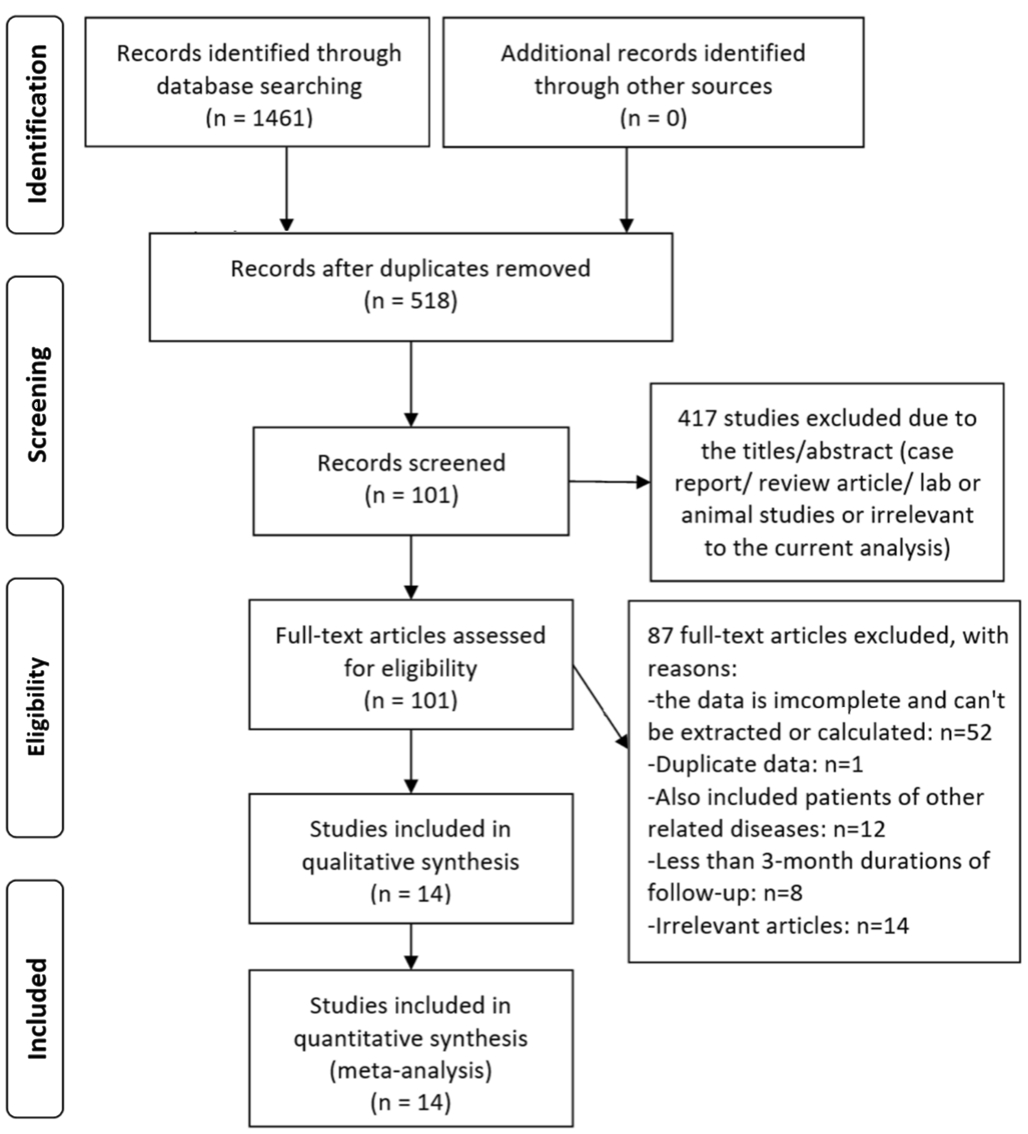
Selection of StudiesA total of 1461 articles were initially identifed.We filtered titles and abstracts of these for potentially relevant articles, 1447 publications were excludedfollowing the selection criteria and a total of 14 studies[10-23]were eligible for this Meta-analysis.The search process is illustrated in Figure 1.
Table 1 Characteristics of the included trials

P: Pars plana vitrectomy alone; I: ILM peeling; CMT: Central macular thickness; BCVA: Best corrected visual acuity.
Studies Group No.of eyes Mean age(y)Preop.BCVA(logMAR)Preop.CMT (μm)Postop.BCVA(logMAR)VA improvement(n/total)Postop.CMT (μm)CMT reduction(n/total)Liu and Sun[16]P 16 58 -- -- -- 10/16 393.00 9/16 P+I 15 58 -- -- -- 14/15 319.00 14/15 Suet al[12]P 30 51.67±6.87 0.86±0.13 439.81±165.21 0.54±0.33 17/30 210.04±76.50 20/30 P+I 30 50.88±6.77 0.92±0.11 513.31±149.02 0.46±0.26 25/30 189.69±56.47 28/30 Luanet al[15]P 23 -- 0.76±0.17 -- 0.48±0.27 7/23 -- --P+I 25 -- 0.77±0.12 -- 0.48±0.29 9/25 -- --Bahadiret al[22]P 41 51.52±11.54 1.22±0.52 -- 0.83±0.44 23/41 --P+I 17 59.60±8.50 1.15±0.31 -- 0.76±0.36 9/17 --Yamamotoet al[10]P 15 58.60±9.90 0.77±0.35 415.70±127.50 0.52±0.44 9/15 191.70±121.60 13/15 P+I 15 61.90±9.40 0.78±0.38 506.50±192.90 0.56±0.34 7/15 253.50±183.60 12/15 Kumagaiet al[17]P 58 61.30±8.80 0.55±0.41 -- 0.43±0.38 28/58 -- --P+I 58 61.30±8.80 0.55±0.31 -- 0.35±0.35 36/58 -- --Stefaniotouet al[13]P 18 65.06±5.30 -- -- -- 8/18 -- --P+I 55 63.75±6.58 -- -- -- 38/55 -- --Hoeraufet al[20]P 19 66.00±8.96 0.59±0.23 425.25±83.25 0.78±0.34 1/19 415.20±132.25 --P+I 20 63.55±7.14 0.59±0.23 442.13±83.73 0.64±0.21 1/20 532.62±102.38 --Kanget al[18]P 10 -- 0.13±0.04 509.50±36.77 0.12±0.03 3/10 332.60±91.73 --P+I 6 -- 0.15±0.09 516.17±55.43 0.14±0.06 2/6 333.83±51.64 --Aboutable[23]P 10 -- 0.78 623.00 0.60 5/10 311.00 --P+I 10 -- 0.74 618.00 0.45 5/10 265.00 --Kamuraet al[19]P 66 58.90±10.30 0.76±0.31 -- 0.43±0.19 -- -- --P+I 34 57.70±9.20 0.73±0.31 -- 0.47±0.18 -- -- --Figueroaet al[21]P 11 68.00±13.32 0.68±0.17 -- 0.74±0.16 -- -- --P+I 20 65.00±9.54 0.59±0.13 -- 0.49±0.22 -- -- --Shibaet al[14]P 66 58.90 0.76 -- 0.69 -- -- --P+I 62 60.50 0.73 -- 0.66 -- -- --Yamakoshiet al[11]P 42 59.80±10.70 0.71±0.32 -- 0.64±0.37 -- -- --P+I 65 61.25±7.30 0.71±0.34 -- 0.50±0.36 -- -- --
Characteristics of the Included StudiesIn total 14 studies[10-23],857 eyes with DME (432 eyes with ILM peeling, 425 eyes with no ILM peeling) were included.Among the 14 studies,8 studies[11,13-15,17-19,23]were nonrandomized trials and 6 studies[10,12,16,20-22]were RCTs.Two studies[12,16]were conducted in China, six in Japan[10-11,14-15,17,19], two in Germany[20,23]and one of each from Turkey[22], Greece[13], Korea[18]and Spain[21],respectively.The characteristics are listed in Table 1.
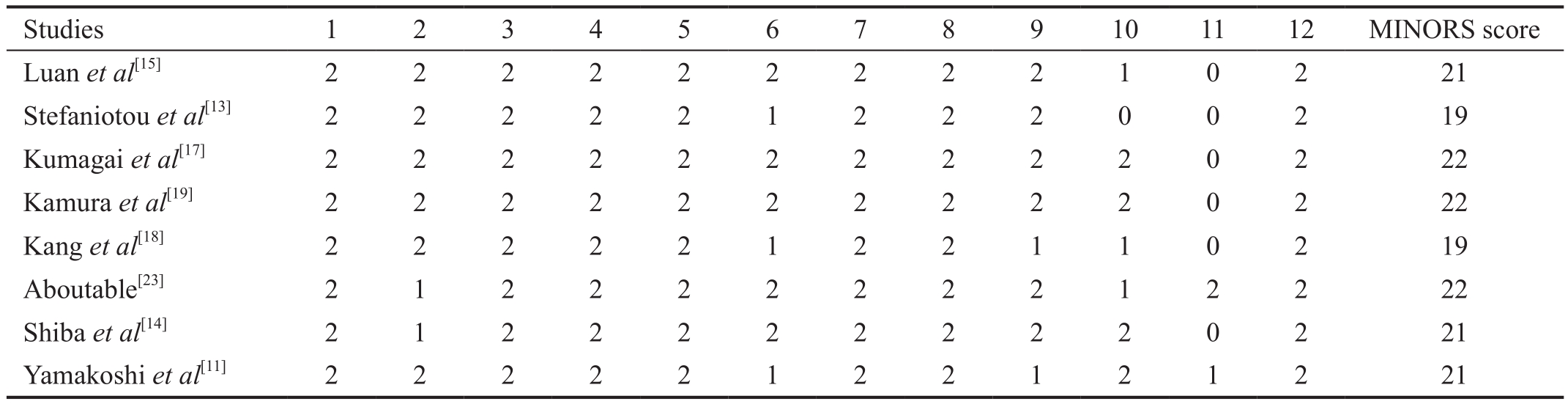
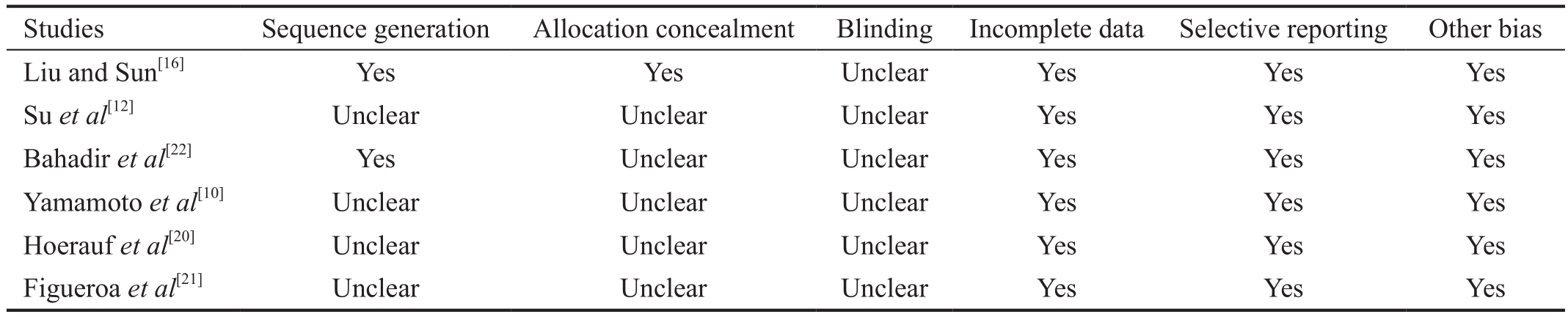
Quality AssessmentAmong the 14 studies, 8 studies[11,13-15,17-19,23]were nonrandomized trials and 6 studies[10,12,16,20-22]were RCTs.Table 2 shows the MINORS[7]scores for the quality of nonrandomized studies.All nonrandomized studies scored ≥18 were identifed as high quality.Other RCTs were assessed under the Cochrane Collaboration Reviewers’ Handbook[8].The opinion about each item of bias risk for included RCTs is illustrated in Table 3, where most of items were at ‘‘low risk’’ based on Cochrane handbook, indicating that RCTs are of good quality.
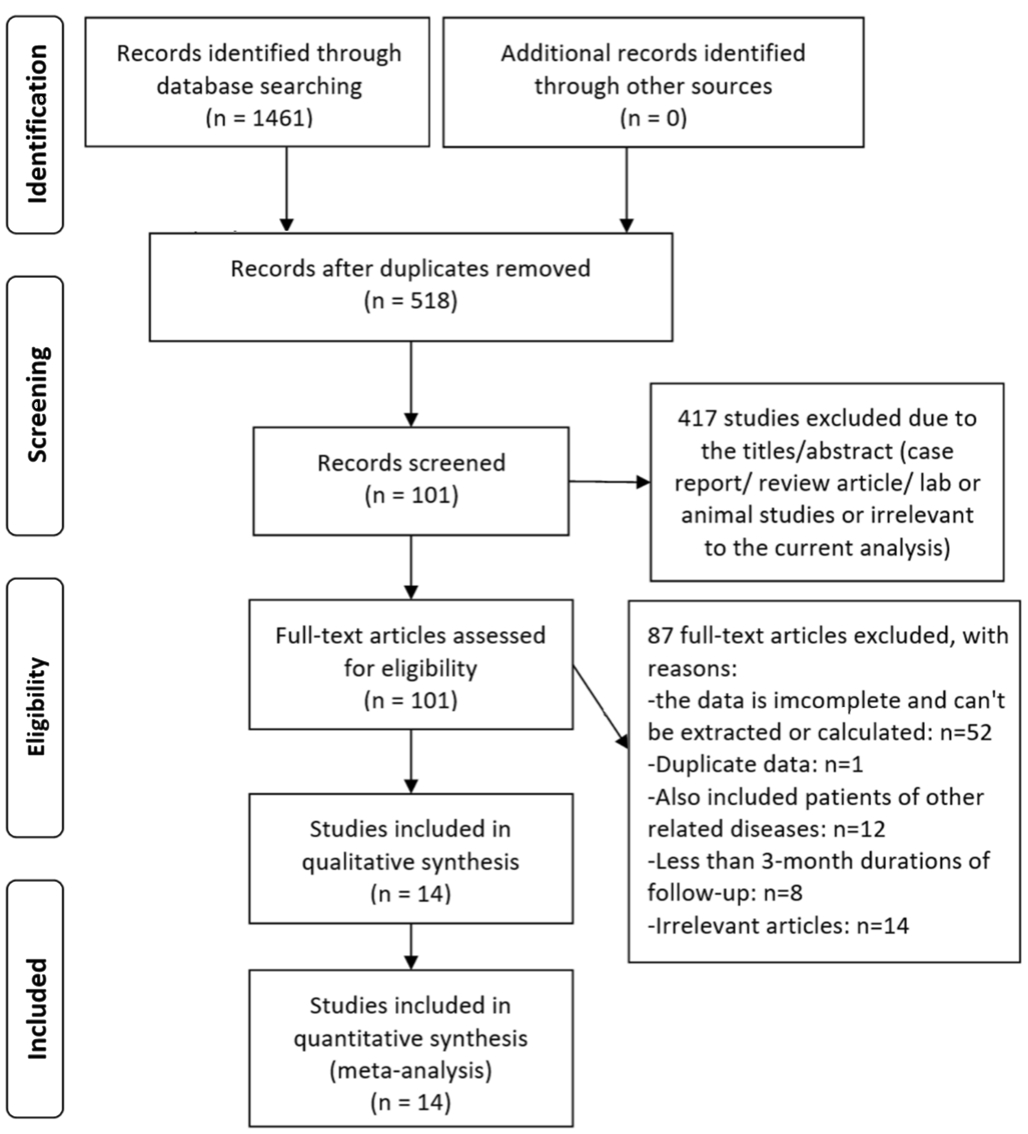
Figure 1 Flow diagram of the process of identifying eligible studies.
Table 2 Quality assessment using the methodological index for nonrandomized studies
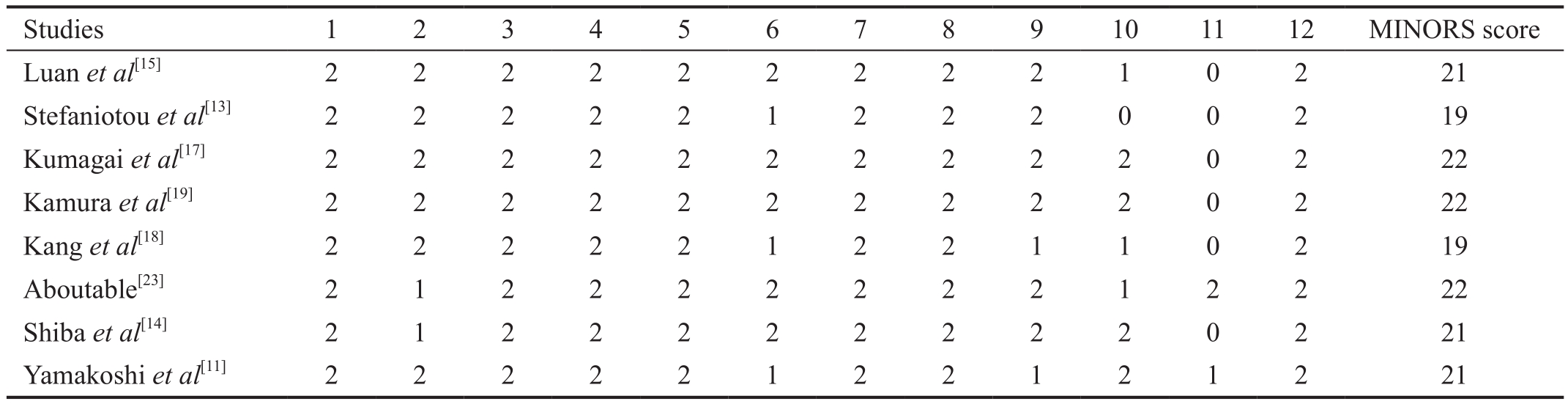
0: Not reported; 1: Reported but inadequate; 2: Reported and adequate.
Studies 1 2 3 4 5 6 7 8 9 10 11 12 MINORS score Luanet al[15]2 2 2 2 2 2 2 2 2 1 0 2 21 Stefaniotouet al[13]2 2 2 2 2 1 2 2 2 0 0 2 19 Kumagaiet al[17]2 2 2 2 2 2 2 2 2 2 0 2 22 Kamuraet al[19]2 2 2 2 2 2 2 2 2 2 0 2 22 Kanget al[18]2 2 2 2 2 1 2 2 1 1 0 2 19 Aboutable[23]2 1 2 2 2 2 2 2 2 1 2 2 22 Shibaet al[14]2 1 2 2 2 2 2 2 2 2 0 2 21 Yamakoshiet al[11]2 2 2 2 2 1 2 2 1 2 1 2 21
Table 3 Quality assessment using Cochrane handbook for randomized controlled studies
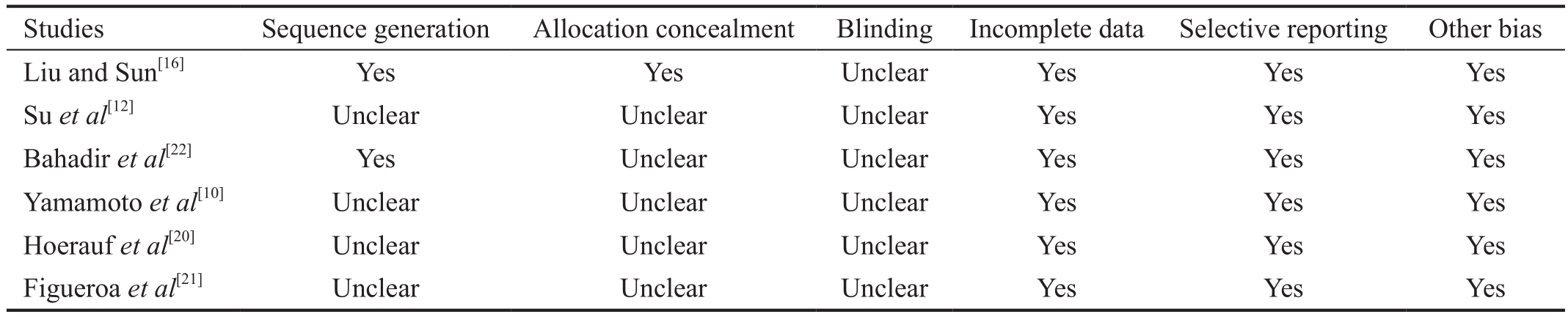
Yes: Low risk of bias; Unclear: Uncertain of bias.
Studies Sequence generation Allocation concealment Blinding Incomplete data Selective reporting Other bias Liu and Sun[16]Yes Yes Unclear Yes Yes Yes Suet al[12]Unclear Unclear Unclear Yes Yes Yes Bahadiret al[22]Yes Unclear Unclear Yes Yes Yes Yamamotoet al[10]Unclear Unclear Unclear Yes Yes Yes Hoeraufet al[20]Unclear Unclear Unclear Yes Yes Yes Figueroaet al[21]Unclear Unclear Unclear Yes Yes Yes
Meta-analysis of Efficacy Analysis
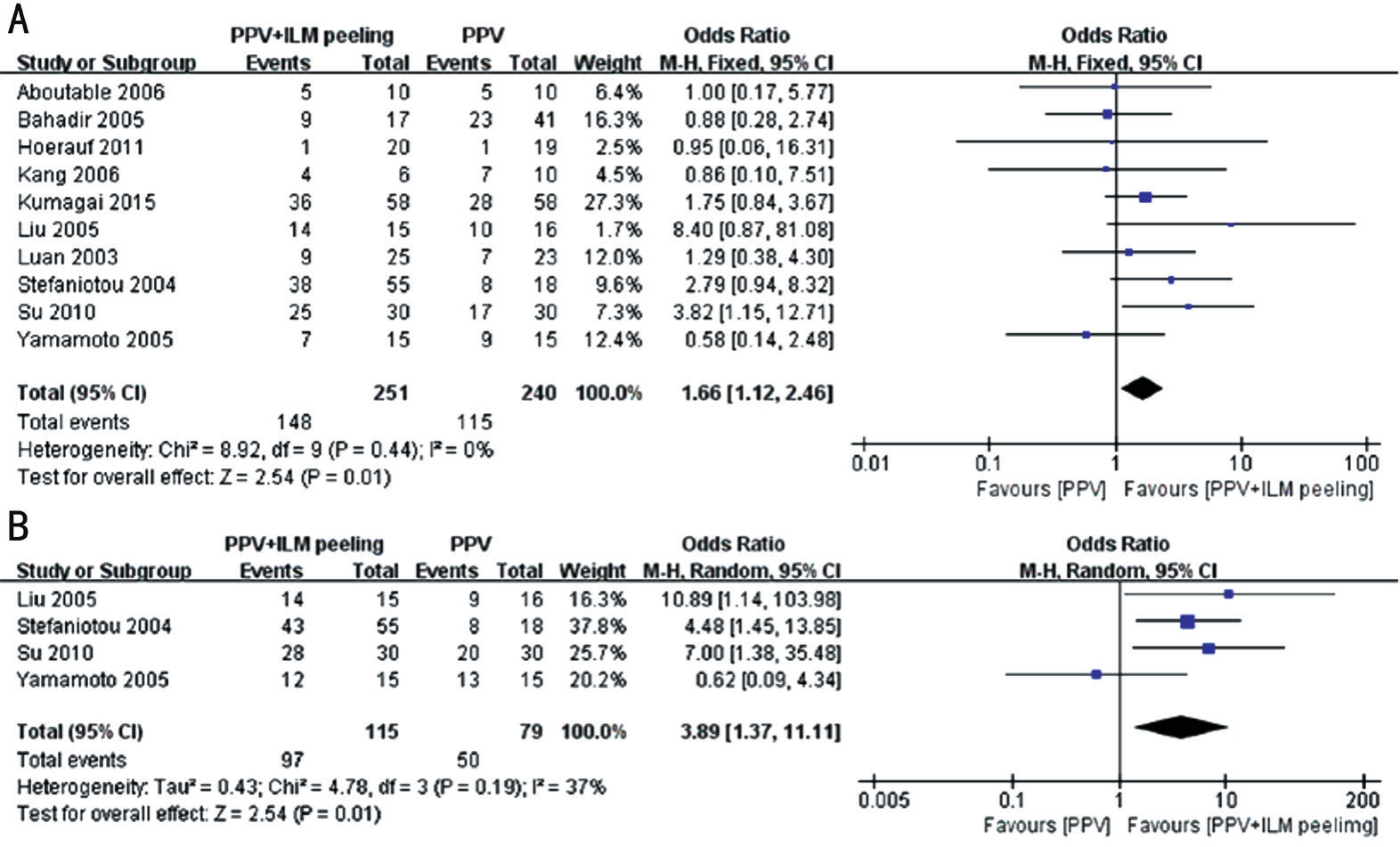
Visual acuityTen studies[10,12-13,15-18,20,22-23]including 491 eyes reported the rate of VA improvement.Besides Stefaniotouet al[13]and Hoeraufet al[20]judged VA improvement by an improvement in VA of ≥3 Snellen lines, other studies defined VA improvement by an improvement in VA of ≥2 Snellen lines.There was no statistical heterogeneity between the studies included (heterogeneityP=0.44,I2=0).Figure 2 shows the results of a Meta-analysis comparing the rate of VA improvement between the ILM peeling and non-peeling groups which indicated that the group of vitrectomy combined with ILM peeling had higher rate of VA improvement than the group of vitrectomy alone.Signifcant difference was detected between the two groups (OR=1.66, 95%CI: 1.12-2.46,P=0.01).Compared with vitrectomy alone, VA could be improved by additional ILM peeling by 66.0%.
Central macular thicknessCMT reduction rates after surgery were reported in 4 studies[10,12-13,16]including 194 eyes.Yamamotoet al[10]judged macular edema absorption by a standard of CMT reduction >20% confirmed by optical coherence tomography (OCT), Stefaniotouet al[13]established macular edema absorption by fuorescence fundus angiography, other studies defned macular edema absorption by OCT confrming CMT reduction >100 μm.There was mild statistical heterogeneity among the studies (heterogeneityP=0.19,I2=37%) which may originated from variations in the standard used to judge macular edema absorption.By using a random-effects model,it indicated that ILM peeling group could increase the CMT reduction rate nearly three times than the group of vitrectomy without ILM peeling and the difference was significant between the two groups (OR=3.89, 95%CI: 1.37-11.11,P=0.01; Figure 2).
Meta-analysis of Safety OutcomesCompared with simple vitrectomy, ILM peeling with vitrectomy may add the diffculty of surgery and increase complication incidents.Ten studies[10-11,13-14,17-21]reported intraoperative and postoperative complications such as iatrogenic peripheral retinal break,epiretinal membrane (ERM), increased intraocular pressure(IOP), central retinal vein occlusion, neovascular glaucoma,vitreous hemorrhage and so on.We analyzed the incidence of complications overall and iatrogenic peripheral retinal break,ERM, increased IOP respectively.It is worth noting that, the heterogeneity test showed no signifcant heterogeneity between the two groups in terms of overall and single complications(heterogeneityP>0.05).As is shown in Figure 3, we analyzed the incidence of overall complications and the results revealed that the two groups did not differ significantly in the regard of applying the fxed effects model (OR=1.19, 95%CI: 0.82-1.73,P=0.36).Although the incidences of iatrogenic peripheral retinal break, ERM and increased IOP indicated no signifcant statistical differences between the two groups (OR=1.21,95%CI: 0.66-2.21,P=0.53; OR=0.38, 95%CI: 0.07-2.00,P=0.25; OR=1.34, 95%CI: 0.75-2.40,P=0.32), the incidence of ERM was slightly lower in the ILM peeling group than the group of vitrectomy without ILM peeling.
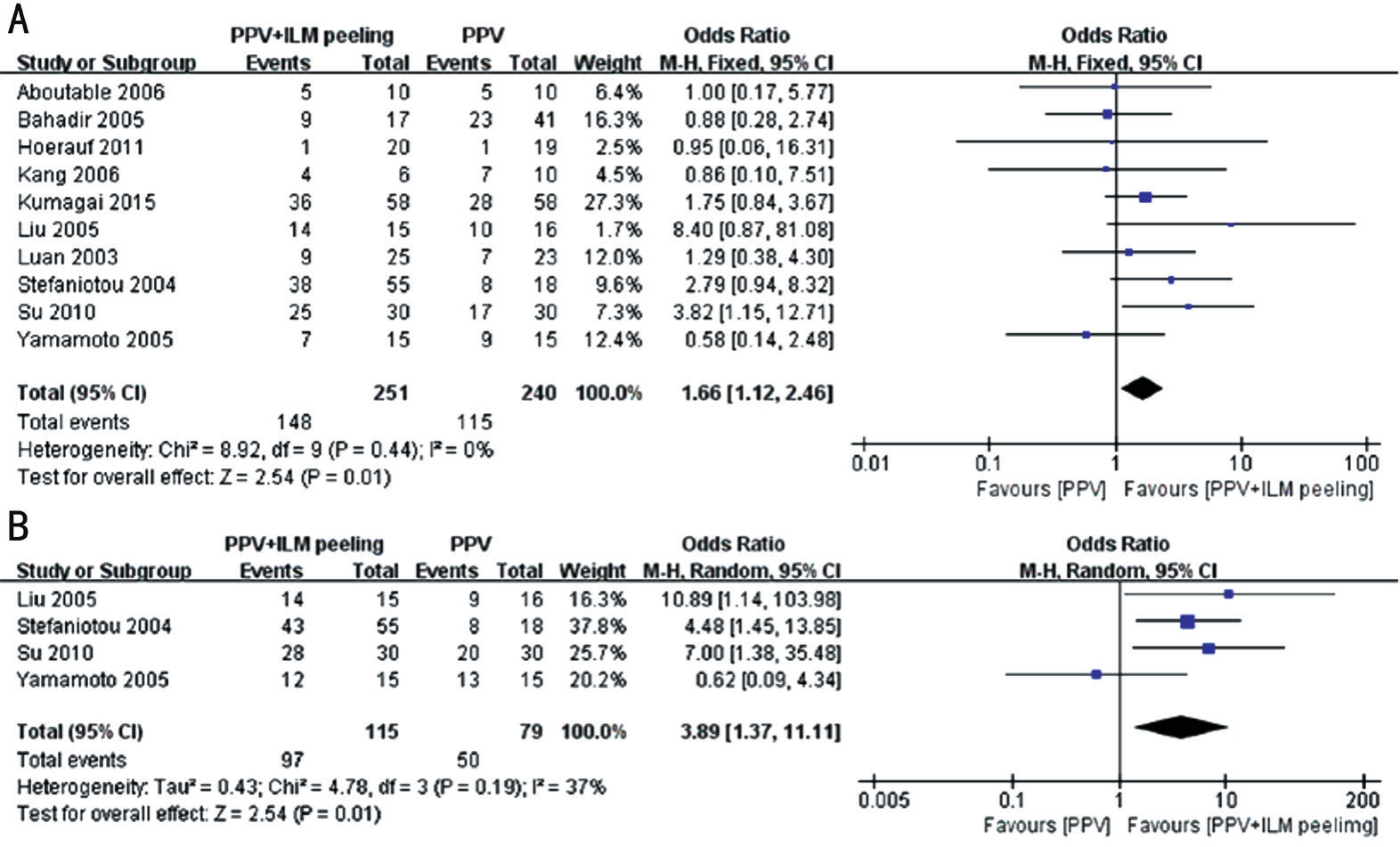
Figure 2 A forest plot shows the rate of VA improvement and CMT reduction between vitrectomy with the ILM peeling and non-peeling groups A: VA improvement; B: CMT reduction.

Figure 3 A forest plot shows the incidence of complications between vitrectomy with the ILM peeling and non-peeling groups A: Overall complications; B: Iatrogenic peripheral retinal break; C: ERM; D: Increased IOP.

Figure 4 Funnel plots of the publication bias analysis A: The rate of VA improvement; B: The rate of CMT reduction; C: The incidence of overall complications; D: The incidence of iatrogenic peripheral retinal break; E: The incidence of ERM; F: The incidence of increased IOP.
Publication Bias and HeterogeneityAs shown in Figure 4,Begg’s funnel plots of the rate of VA improvement, CMT reduction, overall and single complications demonstrated symmetry.Egger’s test was also carried out andPvalue were 0.761, 0.863, 0.665, 0.377, 0.053, 0.466, respectively, which indicated no statistically signifcant evidence (P>0.05) of publication bias was detected.Heterogeneity was evaluated by calculating theI2statistic as well as Chi-square test.I2statistics were 0.0 (P=0.44), 37.0% (P=0.19), 0.0 (P=0.59),0.0 (P=0.73), 0.0 (P=0.72), 0.0 (P=0.68), which indicated no serious heterogeneity between the two groups.
DISCUSSION
This study, to the best of our knowledge, is the first Metaanalysis that evaluates both effcacy and safety of ILM peelingvsno peeling for DME.We reviewed fourteen comparative studies[10-23]involving 857 eyes.The pooled outcomes from our Meta-analys indicated that ILM-peeled group obtained higher rates of vision improvement (OR=1.66, 95%CI: 1.12-2.46,P=0.01) and CMT reduction (OR=3.89, 95%CI: 1.37-11.11,P=0.01).Additionally, the incidence of ERM was slightly lower in the ILM peeling group than the group of vitrectomy without ILM peeling (OR=0.38, 95%CI: 0.07-2.00,P=0.25),although no signifcant statistical differences for the incidences of overall and single complications were detected between the two groups.This study provides important fndings that may help in the selection of surgical maneuvers.
The prevalence of DM is globally increasing with a fast speed.As shown by data, DM had affected 285 million adults in 2010[24], and this figure is expected to increase to 439 million by 2030[24].Therefore, the prevalence of DME and visual impairment caused by DME is expected to increase substantially over time.DME, a diabetes-related ocular disease,is defned as an abnormal thickening of the macular associated with the accumulation of excess fuid in the extracellular space of the neurosensory retina[25].The pathogenesis of DME is multifactorial: diabetes duration, insulin use or not, cardiac and renal failure, high blood pressure, obesity, high glycosylated hemoglobin, proteinuria and panretinal photocoagulation are implicated[26].In the past few years, many therapies for DME have been proposed, such as focal/grid laser photocoagulation,ocular steroids, intravitreal anti-VEGF drugs and vitreoretinal surgery.Before the availability of anti-VEGF therapy, laser photocoagulation therapy was the standard treatment.
Laser photocoagulation may be beneficial when macular edema appears, however, some scholars have reported that there are patients with DME who did not respond to laser therapy[27-28].Nowadays, anti-VEGF therapy is the frst choice for the treatment of DME[29].VEGF plays a key role in the development of DME.A decade of clinical trials demonstrated that, drugs binding soluble VEGF could restore the bloodretinal barrier integrity, resolve macular edema, and improve the vision of most patients with DME.Intravitreal administration of anti-VEGF substances is definitely considered to be the second pivotal breakthrough in the treatment of DME after laser photocoagulation[30].Nevertheless, there are some unanswered questions about anti-VEGF drugs.First, so far,there is lack of data on potential side effects, especially in the long-term period[31].Second, some patients reported did not respond to laser or anti-VEGF substances.Third, effective treatment requires repeated injections which can be a big burden for both patients and ophthalmologists while the risk of recurrence is inevitable.Like anti-VEGFs, steroids(fuocinolone, dexamethasone or triamcinolone) are also aimed at reducing vascular leak in macular with more complications such as secondary IOP rise and cataract but could not avoid the restrictions mentioned above[32].For these reasons, an effective and non-repetitive treatment is needed.Vitreoretinal surgery can surely solve the question for laser-insensitive patients or patients did not respond to anti-VEGF or steroids substances and is the last method for the therapy of refractory DME.
Many studies have demonstrated the efficacy of vitrectomy with ILM peeling for DME.While the use of ILM peeling during PPV for DME remains controversial.Gandorferet al[6]suggested that ILM peeling led to an earlier and greater decrease of retinal thickness or to an earlier and better VA and can decrease the risk of subsequent ERM formation by eliminating a scaffold for proliferating cells.In contrast,Yamamotoet al[10]considered that the removal of the ILM in itself cannot lead to a better resolution of the DME.
Our Meta-analysis is the second, as per our knowledge, to provide statistical results by comparing the VA improvement and CMT reduction to evaluate the effect of PPV with and without ILM peeling for DME.Different from the previous Meta-analysis[33], better functional outcomes and additional safety outcomes were detected in this study, which was the characteristic of this study.Reasons led to the different results between this study and the previous Meta-analysis may be multifactorial.Besides the different indexs to evaluate VA improvement, the duration of diabetic, time of surgery, followup duration, levels of glycosylated hemoglobin and different surgeons may also be influential factors for the final visual outcomes in DME.In addition, it may take longer time to observe the effcacy of ILM peeling on vision, but long-term follow-up studies are largely missing.
It is worthy noting that, when considering the results, the relatively limited powers of our Meta-analysis should not be ignored.Firstly, this study was limited by the low quality of the retrospective studies included.Most of the RCTs did not show sequence generation, allocation concealment or double blinding and were carried out with small sample size.This could compromise the effcacy of this instrument in controlling potential biases.Secondly, results of CMT reduction rate were only obtained from four studies, which may restrict its reliability.Thirdly, in each study, the follow-up duration was different, which may also lead to differences and corresponding biases.Therefore, the interpretation of the results could be affected.Finally, this study was limited to the use of published index, so papers, especially those published in languages other than English and Chinese, may not be included.However, in this study, we had the detailed plan before starting this analysis,the explicit standards for trials selection, and the accurate data extraction, which helped to minimize the likelihood of bias.
Leaving the limitations aside, we believe that the results of this Meta-analysis are credible.Vitrectomy is effective for DME and the effect can be improved by additional ILM peeling.In addition, ILM peeling could reduce the incidence of ERM, although the difference is insignifcant statistically.Furthermore, the lack of prospective randomized study demands more study and evaluation in the future.
ACKNOWLEDGEMENTS
Conflicts of Interest:Hu XY, None; Liu H, None; Wang LN,None; Ding YZ, None; Luan J, None.
REFERENCES
1 Musat O, Cernat C, Labib M, Gheorghe A, Toma O, Zamfr M, Boureanu AM.Diabetic macular edema.Rom J Ophthalmol2015;59(3):133-136.
2 Klein R, Klein BE, Moss SE.Visual impairment in diabetes.Ophthalmology1984;91(1):1-9.
3 Semeraro F, Morescalchi F, Duse S, Gambicorti E, Russo A, Costagliola C.Current trends about inner limiting membrane peeling in surgery for epiretinal membranes.J Ophthalmol2015;2015:671905.
4 Kokame GT.Ultrastructural features of tissue removed during idiopathic macular hole surgery.Am J Ophthalmol1997;123(3):425-426.
5 Stolba U, Binder S, Gruber D, Krebs I, Aggermann T, Neumaier B.Vitrectomy for persistent diffuse diabetic macular edema.Am J Ophthalmol2005;140(2):295-301.
6 Gandorfer A, Messmer EM, Ulbig MW, Kampik A.Resolution of diabetic macular edema after surgical removal of the posterior hyaloid and the inner limiting membrane.Retina2000;20(2):126-133.
7 Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J.Methodological index for non-randomized studies (minors): development and validation of a new instrument.Anz J Surg2003;73(9):712-716.
8 Higgins JP, Green S.Cochrane handbook for systematic reviews of interventions version 5.1.0.Oxford, UK: The Cochrane Collaboration 2011.
9 Higgins JP, Thompson SG, Deeks JJ, Altman DG.Measuring inconsistency in Meta-analyses.BMJ2003;327(7414):557-560.
10 Yamamoto T, Hitani K, Sato Y, Yamashita H, Takeuchi S.Vitrectomy for diabetic macular edema with and without internal limiting membrane removal.Ophthalmologica2005;219(4):206-213.
11 Yamakoshi T, Kachi S, Sugita J, Asami T, Ishikawa K, Ito Y, Terasaki H.Triamcinolone-assisted removal of internal limiting membrane enhances the effect of vitrectomy for diabetic macular edema.Ophthalmic Res2009;41(4):203-209.
12 Su JL, Zheng JQ, Su KX, Shen DL, Ma J.Study on the treatment of diabetic macular edema by striking membrane stripping.Chinese Journal of Trauma and Disability Medicine2010;18(4):34-36.
13 Stefaniotou M, Aaspiotis M, Kalogeropoulos C, Christodoulou A,Psylla M, Ioachim E, Alamanos I, Psilas K.Vitrectomy results for diffuse diabetic macular edema with and without inner limiting membrane removal.Eur J Ophthalmol2004;14(2):137-143.
14 Shiba T, Kamura Y, Yagi F, Sato Y.Comparison of surgical procedures for vitreous surgery in diabetic macular edema.Jpn J Ophthalmol2009;53(2):120-124.
15 Luan J, Ando F, Hiroshe H, Yasui O.ILM peeling for treatment of diabetic macular edema.Chin J Ocul Fundus Dis2003;19(6):343.
16 Liu Z, Sun P.Effcacy of retinal inner membrane peeling in the treatment of diabetic macular edema.Chin J Ocul Fundus Dis2005;21(3):138-141.
17 Kumagai K, Hangai M, Ogino N, Larson E.Effect of internal limiting membrane peeling on long-term visual outcomes for diabetic macular edema.Retina2015;35(7):1422-1428.
18 Kang S, Yoon S, Chin H, Moon Y.The effectiveness of internal limiting membrane peeling on vitrectomy patients with diabetic macular edema.Invest Ophthalmol Vis Sci2006;47(13):995.
19 Kamura Y, Sato Y, Isomae T, Shimada H.Effects of internal limiting membrane peeling in vitrectomy on diabetic cystoid macular edema patients.Jpn J Ophthalmol2005;49(4):297-300.
20 Hoerauf H, Bruggemann A, Muecke M, Lüke J, Müller M, Stefansson E, Hammes HP, Weiss C.Pars plana vitrectomy for diabetic macular edema.Internal limiting membrane delamination vs posterior hyaloid removal.A prospective randomized trial.Graefes Arch Clin Exp Ophthalmol2011;249(7):997-1008.
21 Figueroa MS, Contreras I, Noval S.Surgical and anatomical outcomes of pars plana vitrectomy for diffuse nontractional diabetic macular edema.Retina2008;28(3):420-426.
22 Bahadir M, Ertan A, Mertoglu O.Visual acuity comparison of vitrectomy with and without internal limiting membrane removal in the treatment of diabetic macular edema.Int Ophthalmol2005;26(1-2):3-8.
23 Aboutable T.Is removal of internal limiting membrane always necessary during surgery for refractory diffuse diabetic macular edema without evident epimacular proliferation?KlinMonblAugenheilkd2006;223(8):681-686.
24 Shaw JE, Sicree RA, Zimmet PZ.Global estimates of the prevalence of diabetes for 2010 and 2030.Diabetes Res Clin Pract2010;87(1):4-14.
25 Cai L, Xu GX.Risk factors and the current pharmacotherapy situation of diabetic macular edema.Guoji Yanke Zazhi (Int Eye Sci)2015;15(2):228-232.
26 Jeng CJ, Hsieh YT, Yang CM, Yang CH, Lin CL, Wang IJ.Diabetic retinopathy in patients with diabetic nephropathy: development and progression.PLoS One2016;11(8):e0161897.
27 Ulrich JN.Pars plana vitrectomy with internal limiting membrane peeling for nontractional diabetic macularedema.Open Ophthalmol J2017;11:5-10.
28 Massin P, Haouchine B, Gaudric A.Macular traction detachment and diabetic edema associated with posterior hyaloidal traction.Am J Ophthalmol2001;132(4):599-600.
29 Stewart MW.Anti-VEGF therapy for diabetic macular edema.Curr Diab Rep2014;14(8):510.
30 Bandello F, Berchicci L, La Spina C, Battaglia Parodi M, Iacono P.Evidence for anti-VEGF treatment of diabetic macular edema.Ophthalmic Res2012;48 Suppl 1:16-20.
31 Bandello F, Cunha-Vaz J, Chong NV, Lang GE, Massin P, Mitchell P,Porta M, Prunte C, Schlingemann R, Schmidt-Erfurth U.New approaches for the treatment of diabetic macular oedema: recommendations by an expert panel.Eye (Lond)2012;26(4):485-493.
32 Amoaku WM, Saker S, Stewart EA.A review of therapies for diabetic macular oedema and rationale for combination therapy.Eye(Lond)2015;29(9):1115-1130.
33 Nakajima T, Roggia MF, Noda Y, Ueta T.Effect of internal limiting membrane peeling during vitrectomy for diabetic macular edema:systematic review and Meta-analysis.Retina2015;35(9):1719-1725.
Citation:Hu XY, Liu H, Wang LN, Ding YZ, Luan J.Efficacy and safety of vitrectomy with internal limiting membrane peeling for diabetic macular edema: a Meta-analysis.Int J Ophthalmol2018;11(11):1848-1855
DOl:10.18240/ijo.2018.11.18
Accepted:2018-05-25
Received:2018-03-25
Correspondence to:Jie Luan.Department of Ophthalmology,Zhongda Hospital, Southeast University, 87 Dingjiaqiao Road,Gulou District, Nanjing 210009, Jiangsu Province, China.luanqiu10@163.com