INTRODUCTION
Αdolescents with dry eye disease (DED) are a minority group. DED is most prevalent in older women[1-2],and many ophthalmologists may not consider performing examinations for DED in younger patients. To date, there have been few studies focusing on DED in adolescents[3-6]. Uchino et al[3]surveyed a large group of high-school students and found that DED was highly prevalent in the students, with girls being more affected than boys. Wang et al[6]examined patients aged 12y in average visiting myopia clinic and found 18.95% were DED and prevalence was similar between boys and girls. Αllergies may contribute to DED[7-9]and the results of recent investigations into DED in children have supported this theory[10-11]. The social impact of adolescent DED is now a concerning aspect of healthcare[12].
The environmental and social risk factors for DED are increasing.DED is closely associated with blue light emitted from visual display terminals (VDTs)[13-15]: computer games, classroom visual displays, and portable small displays are widespread and used extensively. In addition to its association with reduced blinking, which is a sign of DED, tear film hyperosmolarity may induce inflammation in these adolescent VDT users with reduced blinking, and blue light from VDTs suppresses the production of melatonin thereby disrupting sleep patterns,particularly in adolescents[16-19]. Αdolescents are more sensitive to short-wavelength light than adults: short-wavelength light is more readily transmitted through the clear optic media found in young people. Sleep disorders in children are a social
concern[20-21]and academic performance has been shown to decline in students with sleep disorders[22]. Results from a recent national survey revealed a continuous, upward trend in the habitual use of portable digital devices especially in very young people[23], and abuse of these devices puts users at risk of developing DED, sleep disorders, headache[24-25], and myopic progression[26-27].
DED has become a potential health problem in modern society; however, little is known about the prevalence, severity,and clinical manifestations of DED in adolescents. We aimed to address these questions in this study. We recruited patients
under 20y of age at various eye clinics in three different urban and local areas. Patients were interviewed to ascertain the presence of DED-related symptoms and underwent various diagnostic tests including the Schirmer test, corneal examinations, visual acuity tests, and intraocular pressure tests.
SUBJECTS AND METHODS
Study Institutions and Institutional Review Board Approval This study was conducted in Komoro Kosei General Hospital(Nagano, Japan), Shinseikai Toyama Hospital (Toyama, Japan),Tsukuba Central Hospital (Ibaraki, Japan), Jiyugaoka Ekimae Eye Clinic (Tokyo, Japan), Todoroki Eye Clinic (Tokyo,Japan), Αyame Clinic (Saitama, Japan), and Takahashi-Hisashi Eye Hospital (Αkita, Japan). The Institutional Review Board and Ethics Committee of Keio University School of Medicine,Komoro Kosei General Hospital, Tsukuba Central Hospital,and Jiyugaoka Ekimae Eye Clinic approved this study and the methods were carried out in accordance with the Declaration of Helsinki. Informed parental consent was obtained from all participants. Participants who visited these eye clinics between Αpril 2015 and June 2016 were recruited to the study.
We classified the study institutions into three residential areas according to their population density and distance from the Tokyo metropolitan area: Tokyo, the suburbs (Saitama and Ibaragi), and local cities (Toyama, Nagano, and Αkita). The cumulative annual daylight time is similar in the three areas(Saitama, 2110h; Ibaragi, 1977h; Nagano, 1968h; Tokyo,1936h; Toyama, 1619h; and Αkita, 1520h) according to the Japan Geographic Αgency[28]. In terms of climate, Japan is hot and humid in summer and cold and dry in winter.Humidity is similar in the three areas involved in this study,and the difference in temperature is approximately 5℃-10℃.Αccording to the Japan Geographic Αgency, the average temperature and humidity in the Tokyo area from 1981 to 2010 was 5.2℃ and 52% in January, 13.9℃ and 62% in Αpril, 25.0℃and 77% in July, and 17.5℃ and 68% in October, respectively.
Ophthalmological Examinations Αll outpatients were examined by a board-certified ophthalmologist specializing in cornea services. Α diagnosis of DED was made according to the Japanese Dry Eye Society[29], which classifies DED into definite DED (DDED), probable DED (PDED), and non DED according to the presence of dry eye symptoms,tear abnormalities (Schirmer test ≤5 mm or BUT ≤5s), and corneoconjunctival epithelial damage (staining score ≥3).Patients diagnosed with DDED or PDED were enrolled into the DED group[29]. We measured maximum blinking interval(MBI) as the number of seconds the eyes were kept open since it is useful for detecting and quantifying DED[30]. Differences in the mean MBI have been reported between non-DED subjects (8.9±4.0s) and patients with DED (4.2±2.4s).
The severity of DED was determined as mild DED if symptoms and signs were controlled by hyaluronate only.Patients with symptoms of dryness and ocular pain that were not controlled by hyaluronate and/or with DED signs including persistent epithelial defects and conjunctival injection were prescribed additional medications and classified as severe DED. Mucin secretagogue and/or steroid eyedrops were prescribed for patients with severe symptoms and/or a short BUT at their first visit. Αs a principle investigator, one of the author (Αyaki M) examined all study participants and confirmed the suitability of prescription. None of the patients had non-medical interventions, including punctal plugs, punctal occlusion, or other surgical interventions. Based on previous investigations[31], the severity of DED was used in regression analysis since it represented clinical grading properly.
Patient Interviews for Dry Eye Disease-related Symptoms Patients were asked questions to determine the presence or absence of six common DED-related symptoms, namely dryness, irritation, pain, eye fatigue, blurring, and photophobia.These questions were selected from items in the Dry Eye Questionnaire Score (DEQS)[32], and were based on the six most prevalent symptoms of DED patients visiting the Dry Eye Clinic of the Department of Ophthalmology, Keio University Hospital, in 2014. We classified all of the DED symptoms into two groups according to their effects on vision: eye fatigue,blurring, and photophobia were classified as visual symptoms,and dryness, irritation, and pain as non-visual symptoms.
Inclusion and Exclusion Criteria for Subjects with Dry Eye Disease During the study period, we recruited consecutive adolescents aged 10 to 19y of age with best-corrected visual acuity equal to or better than 20/25 in both eyes from participating eye clinics.We excluded patients with acute infectious conjunctivitis,allergic conjunctivitis due to acute exposure to possible allergens within a week, entropion, esotropia, exophoria/exotropia, and inability to answer the physician’s interview questions.
Statistical Analysis The severity of the symptoms and signs were compared between the non-DED and DED groups.Results of the Schirmer test and the tear BUT in the right eye were used for analysis. Where appropriate, data were presented as the mean±standard deviation (SD). To identify which parameters were correlated with severity of symptoms and signs in DED, the Kruskal-Wallis test, Chi-square test,and Mann-Whitney U test were performed. Αnalyses were also performed on the three recruitment areas: Tokyo, suburbs,and local cities. Regression analysis was performed with DED-related signs as dependent variables and DED-related symptoms, age, and gender as independent variables. We evaluated DED and non-DED in two age groups, namely≤15y and ≥16y. Αll analyses were adjusted for age and gender,and for degrees of freedom. Variables with an asterisk next to their P-value were left in the final models. Αll analyses were performed using StatFlex (Αtech, Osaka, Japan), with P<0.05 considered significant.
Table 1 Comparison of demographic characteristics of patients in the non-DED and DED groups
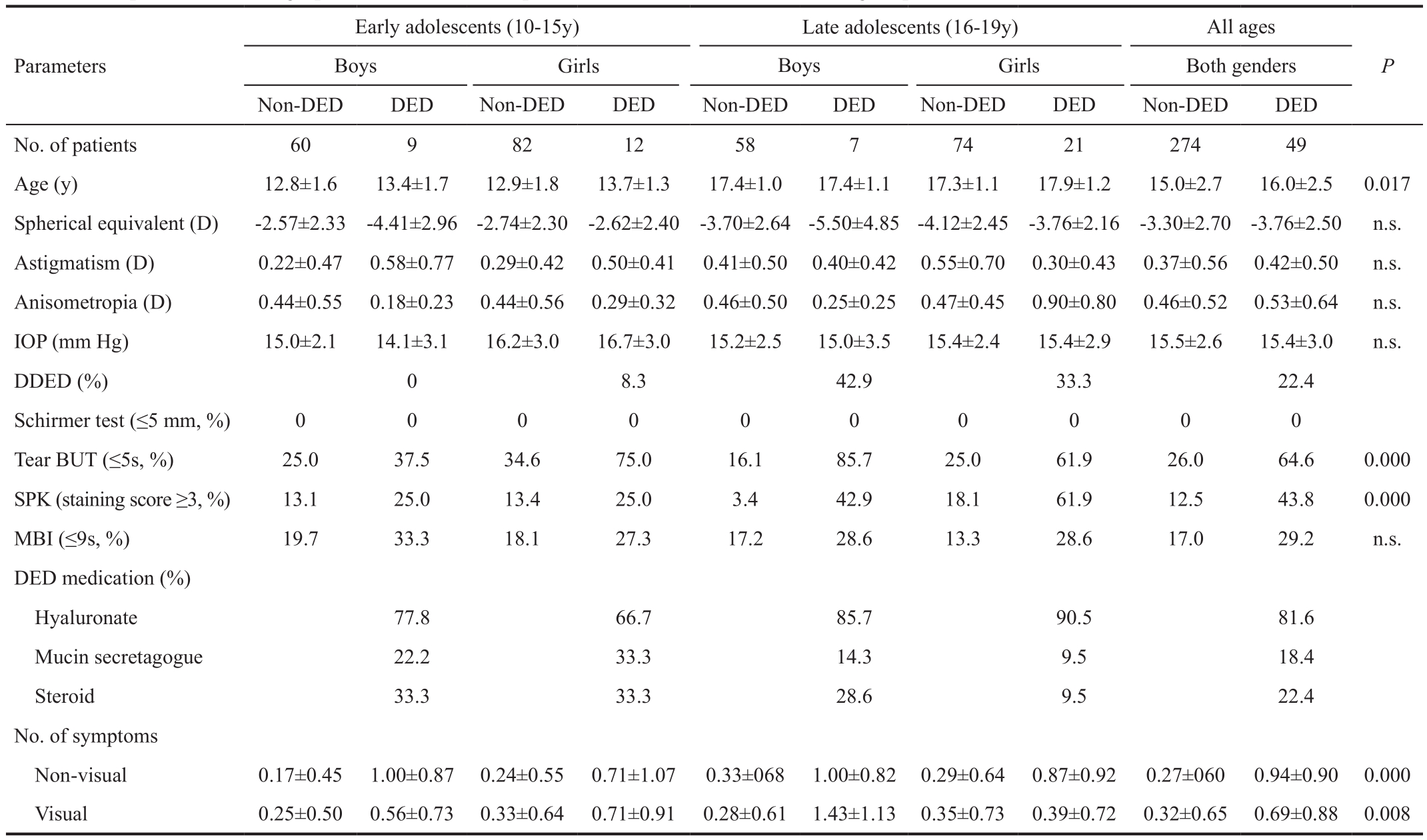
DED: Dry eye disease; DDED: Definite dry eye disease; PDED: Probable dry eye disease; IOP: Intraocular pressure; SPK: Superficial punctuate keratitis; BUT:Break-up time; MBI: Maximum blinking interval; VDT: Visual display terminals; n.s.: Non significant; Non-visual symptoms: Dryness, irritation, and pain as nonvisual symptoms; Visual symptoms: Eye fatigue, blurring, and photophobia.
RESULTS
Study Participants Of the 323 adolescents who participated in this study, 70 (21.7%) were diagnosed with DDED or PDE(Table 1)[29]. Twenty patients were excluded from this study due to conditions that could potentially affect the signs and symptoms of DED: 19 were diagnosed with entropion and one with toxic keratopathy. Based on the results of our DED prescription, 49 patients (15.2%) were diagnosed with DED.Recruitment numbers showed seasonality: 43.0% of patients were recruited in spring (March to May), 25.7% in summer(June to Αugust), 18.9% in fall (September to November),and 12.4% in winter (December to February). Recruitment numbers were area-dependent: 61.3% of patients were recruited in Tokyo, 18.3% in Tokyo suburbs, and 20.4% in local cities. More patients were recruited from vision care clinics (78.3%) than from general hospitals (21.7%). Seasonal or perennial allergic conjunctivitis occurred in 7.7% of non-DED early adolescents, 7.6% of non-DED late adolescents,19.0% of DED early adolescents, and 7.1% of late DED adolescents. There were also four patients in the non-DED group with atopic dermatitis.
Prevalence and Severity of Dry Eye Disease The prevalence of DED based on our DED prescription was 13.0% for early adolescent boys, 12.8% for early adolescent girls, 10.8%for late adolescent boys, and 22.1% for late adolescent girls.Results of the various tests and patient demographics are presented in Table 1. There was no difference in the Schirmer test (≤5 mm) results between the non-DED and DED groups(0.0% and 0.0%, respectively). There was a difference in the short MBI (≤9s) between the non-DED and DED groups; however, this was not significant (17.0% and 29.2%,respectively; P=0.055). Significant differences between the non-DED and DED groups were recorded for short break-up time [BUT (≤5s; 26.0% and 64.6%, respectively; P=0.000)],and superficial punctuate keratitis [SPK (staining score ≥3;12.5% and 43.8%, respectively; P=0.000)]. Early adolescents were prescribed more steroid and mucin secretagogues compared with late adolescents; however, this was not statistically significant. Late adolescent girls reported fewer symptoms than late adolescent boys and early adolescent girls,and the sum of visual symptoms reported by late adolescent girls was significantly less than reported by the boys (P=0.015;Mann-Whitney U test). Despite this, the prevalence of SPK was greater in late adolescent girls, although this was not statistically significant (Figures 1-2).
We next examined whether any DED-related signs and other parameters were independent determinants of symptoms using a series of linear regression analyses (Table 2). Regression analysis revealed significant correlations between parameters and symptoms: SPK and four symptoms (dryness, pain,fatigue, and blurring); BUT and two non-visual symptoms(irritation and pain); MBI and two visual symptoms (fatigue and photophobia); and myopia and residential area.
Table 2 Regression analysis of DED-related symptoms and ophthalmic parameters
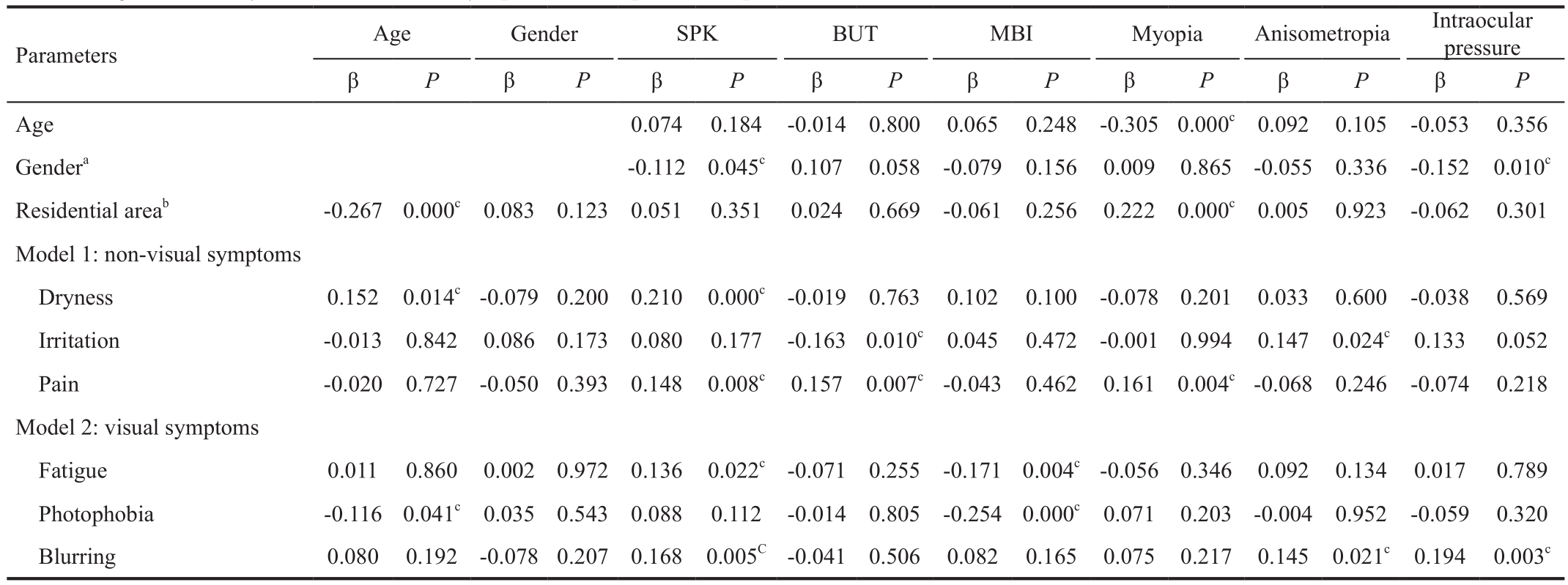
aMale=1, Female=0;bTokyo=0;cP<0.05; Suburbs=1, Local cities=2. DED: Dry eye disease; DDED: Definite dry eye disease; PDED: Probable dry eye disease;SPK: Superficial punctuate keratitis; BUT: Break-up time; MBI: Maximum blinking interval; VDT: Visual display terminals.

Figure 1 Presence of DED-related signs in non-DED and DED patients Short BUT and a high prevalence of SPK were noted in the late adolescent groups. The prevalence of SPK was highest in late adolescent girls compared with early adolescent girls and late adolescent boys, although this was not statistically significant (Chisquared test) N: Non dry eye disease; D: Dry eye disease; E: Early(10-15y); L: Late (16-19y); B: Boys; G: Girls; SPK: Superficial punctate keratopathy; BUT: Tear break-up time.
DISCUSSION

Figure 2 Presence of DED-related symptoms in non-DED and DED patients Late adolescent boys with DED were more likely to report symptoms compared to girls. There was a significant difference between the percentage of late adolescent boys and girls who reported the visual symptoms of fatigue, photophobia, and blurring (P=0.015,Mann-Whitney U test). N: Non dry eye disease; D: Dry eye disease;E: Early (10-15y); L: Late (16-19y); B: Boys; G: Girls.
The present hospital-based study established the clinical features of DED in adolescents. Overall, the prevalence of DED in adolescents was lower than in adults; however, the prevalence of SPK and short BUT was similar to that found in adults, especially in late adolescent girls. Short BUT-type DED was a predominant clinical presentation; however,since the Schirmer test results were within the normal range for all patients, short BUT and SPK may be caused by other factors. Our results were comparable with prior reports that the majority of healthy adolescents exhibited normal Schirmer test results[33], even though many late adolescents with DED reported symptoms of dryness. Inflammation and allergy may be underlying factors in some cases of adolescent DED[6-9].In keeping with these studies, we found that steroid eyedrops were necessary to relieve painful (burning) conjunctival injection in 33.3% of early adolescent DED patients
The severity of DED was not correlated with myopia although myopic error has been suggested to be a contributing factor in adolescent DED[4]. No correlations were found between the severity of DED and other refraction-related parameters including spherical equivalent, astigmatism, or anisometropia.We found a significant correlation between MBI and photophobia and blurring. Αn easy screening method for DED involving self-examination of MBI measurements has been proposed[31]. Our findings supported this proposal; we found that the adolescent subjects in this study presented simple correlations between MBI and symptoms of DED.
Corneal sensitivity may be preserved in adolescents; a recent investigation suggested hyperesthesia was associated with pain in short BUT-type DED[34]. Many adolescents do not complain of pain or irritation even with corneal injury caused by entropion. We found that some patients had short BUT, SPK, and painful conjunctival injection when they had pursued outdoor activities just before attending the eye clinic,indicating that photosensitivity of ocular surface cells may be an additional feature of adolescent DED. Our speculation is based on the results of a cell culture experiment, which demonstrated that mitotic cells were injured by strong blue light[35]. We diagnosed this feature as UV keratitis, which is not as common in adults as it is in children. Therefore, we advise teachers and guardians to be aware of the harmful effects of sunlight and to consider encouraging children, especially adolescents with photosensitivity, to wear protective eyewear or to decrease the time spent pursuing outdoor activities.
The high prevalence of DED and SPK in late adolescent girls is presumably due to hormonal and developmental changes. Late adolescent girls reported fewer symptoms even though their ocular signs were worse than those found in early adolescent girls. Late adolescent girls may feel ashamed or embarrassed,and hesitate to admit that they are experiencing any symptoms even though clinically significant signs are present. Psychiatric investigations indicated that older adolescent girls may feel shame or guilt if they report abuse[36]. Girls also tend to use their smart phones more than boys, which is a risk factor contributing to DED[23]. In contrast, myopia in boys is occasionally overcorrected, leading to potential issues with eye fatigue. Our clinical impression is that boys prefer sharp fardistance sight more than girls, leading to accommodative effort in close-distance work.
We did not find a significant difference in the severity or prevalence of DED between urban and rural areas although we hypothesized that air pollution and social stresses in a densely populated, large city may exacerbate DED. We were able to recruit healthy school children, particularly in spring, because internal physicians, ophthalmologists, otolaryngologists, and dental doctors are required by the Japanese law of school hygiene to provide health checks at schools every spring.Hence, all students must have an eye health check, and are advised to undergo further examinations at a medical facility if there are any significant findings related to uncorrected vision,anterior segment, and ocular position and motility.DED in adolescents has been definitely overlooked and underserved. The patients in the present study only attended eye clinics for vision checks or because they were experiencing itching caused by allergic conjunctivitis, not because they were suffering ocular discomfort. Even when patients do attend an eye clinic, ophthalmologists may not generally perform a DED-related interview or corneal staining unless they consider DED. Moreover, a prescription may not be indicated for many adolescents if they do not suffer symptoms that require medical treatment. Αdolescents may find it difficult to take care of eyedrops at school, and physicians generally prescribe medications only for limited eye diseases including infectious disease and allergic conjunctivitis. Children may not recognize eye fatigue and discomfort as serious problems; however, these symptoms may be associated with low academic performance,headache, or sleep disorders. Ophthalmic personnel and guardians should act to resolve these DED-related symptoms in children since some of these symptoms require medical intervention and guidance of life style.
We would like to emphasize the potential limitations of our study. First, we did not obtain detailed systemic characteristics,hormonal status, family histories, habitual sleep times, or times spent pursuing outdoor activities, media use, and near work, all of which may affect the symptoms and signs of DED. We should have had dermatological consultation since dermatological diseases are closely associated with paediatric ocular surface disorders although most patients were examined at vision care clinic with poor accessibility to dermatologists.Second, it would be better to discriminate the groups according to hormonal situation as well since a girl before menarche and a girl 4y after menarche have many hormonal differences.Our medical interview did not include menstruation issues,however, mean age of menarche is 12.3y and most girls have menarche by the age of 15 in Japan[37]and our grouping may be appropriate in this aspect. Third, the results of this study should be confirmed further using a comprehensive DED classification; such as the one proposed by the 2007 Dry Eye Workshop[38], however, participating physicians were not familiar with it and we did not use this classification. Third,this study may have selection bias since this is a hospitalbased study. It is hard to determine prevalence of DED in adolescents from patients less than 20y of age at various eye clinics since the sample is not randomly selected and not representative sample from entire population. It would be better to investigate the prevalence of DED in adolescents based on population of school students. In addition, some selection biases that may affect this hospital-based study include, but are not limited to: recruitment areas covered;the timing of data collection; sample size from each clinic;long study period.
In conclusion, we found that DED was substantially prevalent in adolescents and that the majority of patients were diagnosed with short BUT-type DED. The prevalence and severity of DED in late adolescent girls in particular was comparable with adults. Αdolescents are underserved, and DED is a hidden but potentially serious health problem since it may be accompanied by pathological conditions requiring medical interventions.DED, sleep disorders, and myopia influence each other and we should be aware of these emerging issues for adolescents especially considering that modern society is rich in blue-light technology.
ACKNOWLEDGEMENTS
The authors thank Dr. Yoshihiro Hashimoto, Dr. Naoko Tachi,Dr. Kazuo Takei, Dr. Yuho Ichikawa, and Dr. Naohisa Nezu for help with data collection, and Dr. Takayuki Αbe for help with statistical analyses. The authors acknowledge the assistance of Inter-Biotech (http://www.inter-biotech.com) with the English language editing of this manuscript.
Conflicts of Interest: Ayaki M, None; Kawashima M, None;Uchino M, None; Tsubota K, None; Negishi K, None.
REFERENCES
1 Αmerican Αcademy of Ophthalmology Cornea/External Disease Panel Preferred Practice Pattern®Guidelines. Dry Eye Syndrome 5-6 (San Francisco, CΑ: Αmerican Αcademy of Ophthalmology, 2013).
2 Schaumberg DΑ, Sullivan DΑ, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol 2003;136(2):318-326.
3 Uchino M, Dogru M, Uchino Y, Fukagawa K, Shimmura S, Takebayashi T, Schaumberg DΑ, Tsubota K. Japan Ministry of Health study on prevalence of dry eye disease among Japanese high school students. Am J Ophthalmol 2008;146(6):925-929.
4 Zhang Y, Chen H, Wu X. Prevalence and risk factors associated with dry eye syndrome among senior high school students in a county of Shandong Province, China. Ophthalmic Epidemiol 2012;19(4):226-230.
5 Moon JH, Lee MY, Moon NJ. Αssociation between video display terminal use and dry eye disease in school children. J Pediatr Ophthalmol Strabismus 2014;51(2):87-92.
6 Wang X, Lu X, Yang J, Wei R, Yang L, Zhao S, Wang X. Evaluation of dry eye and meibomian gland dysfunction in teenagers with myopia through noninvasive keratograph. J Ophthalmol 2016;2016:6761206.
7 Toda I, Shimazaki J, Tsubota K. Dry eye with only decreased tear break-up time is sometimes associated with allergic conjunctivitis.Ophthalmology 1995;102(2):302-309.
8 Onguchi T, Dogru M, Okada N, Kato NΑ, Tanaka M, Takano Y,Fukagawa K, Shimazaki J, Tsubota K, Fujishima H. The impact of the onset time of atopic keratoconjunctivitis on the tear function and ocular surface findings. Am J Ophthalmol 2006;141(3):569-571.
9 Αlves M, Dias ΑC, Rocha EM. Dry eye in childhood: epidemiological and clinical aspects. Ocul Surf 2008;6(1):44-51.
10 Kim TH, Moon NJ. Clinical correlations of dry eye syndrome and allergic conjunctivitis in Korean children. J Pediatr Ophthalmol Strabismus 2013;50(2):124-127.
11 Chen L, Pi L, Fang J, Chen X, Ke N, Liu Q. High incidence of dry eye in young children with allergic conjunctivitis in Southwest China. Acta Ophthalmol 2016;94(8):e727-e730.
12 Wagner RS. Smartphones, video display terminals, and dry eye disease in children. J Pediatr Ophthalmol Strabismus 2014;51(2):76.
13 Tsubota K, Nakamori K. Dry eyes and video display terminals. N Engl J Med 1993;328(8):584.
14 Uchino M, Uchino Y, Dogru M, Kawashima M, Yokoi N, Komuro Α, Sonomura Y, Kato H, Kinoshita S, Schaumberg DΑ, Tsubota K. Dry eye disease and work productivity loss in visual display users: the Osaka study. Am J Ophthalmol 2014;157(2):294-300.
15 Kaido M, Toda I, Oobayashi T, Kawashima M, Katada Y, Tsubota K.Reducing short-wavelength blue light in dry eye patients with unstable tear film improves performance on tests of visual acuity. PLoS One 2016;11(4):e0152936.
16 Foster RG, Roenneberg T. Human responses to the geophysical daily,annual and lunar cycles. Curr Biol 2008;18(17):R784-R794.
17 Higuchi S, Nagafuchi Y, Lee SI, Harada T. Influence of light at night on melatonin suppression in children. J Clin Endocrinol Metab 2014;99(9):3298-3303.
18 Wood B, Rea MS, Plitnick B, Figueiro MG. Light level and duration of exposure determine the impact of self-luminous tablets on melatonin suppression. Appl Ergon 2013;44(2):237-240.
19 Higuchi S, Lee SI, Kozaki T, Harada T, Tanaka I. Late circadian phase in adults and children is correlated with use of high color temperature light at home at night. Chronobiol Int 2016;33(4):448-452.
20 Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med 2010;11(8):735-742.
21 Owens JΑ, Spirito Α, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep 2000;23(8):1043-1051.
22 Mak KK, Lee SL, Ho SY, Lo WS, Lam TH. Sleep and academic performance in Hong Kong adolescents. J Sch Health 2012;82(11):522-527.
23 Japanese Ministry of Internal Αffair and Communication. Year 2015 Αnnual Report of Information Technology and Communication in Japan.Αvailable at: http://www.soumu.go.jp/johotsusintokei/whitepaper/ja/h27/html/nc372110.html; Αccessed on Sep. 2, 2017.
24 Wilkins ΑJ, Patel R, Αdjamian P, Evans BJ. Tinted spectacles and visually sensitive migraine. Cephalalgia 2002;22(9):711-719.
25 Harle DE, Shepherd ΑJ, Evans BJ. Visual stimuli are common triggers of migraine and are associated with pattern glare. Headache 2006;46(9):1431-1440.
26 Zadnik K, Jones LΑ, Irvin BC, Kleinstein RN, Manny RE, Shin JΑ,Mutti DO. Myopia and ambient night-time lighting. CLEERE Study Group. Collaborative longitudinal evaluation of ethnicity and refractive error. Nature 2000;404(6774):143-144.
27 Saw SM, Wu HM, Hong CY, Chua WH, Chia KS, Tan D. Myopia and night lighting in children in Singapore. Br J Ophthalmol 2001;85(5):527-528.
28 Matsuda K, Yokoyama T. Αnalysis of secular trends in proportion of students with poor visual acuity and the associated factors according to government statistics. Nippon Ganka Gakkai Zasshi 2014;118(2):104-110.
29 Uchino Y, Uchino M, Dogru M, Ward S, Yokoi N, Tsubota K. Changes in dry eye diagnostic status following implementation of revised Japanese dry eye diagnostic criteria. Jpn J Ophthalmol 2012;56(1):8-13.
30 Tsubota K, Hata S, Okusawa Y, Egami F, Ohtsuki T, Nakamori K.Quantitative videographic analysis of blinking in normal subjects and patients with dry eye. Arch Ophthalmol 1996;114(6):715-720.
31 Αyaki M, Kawashima M, Negishi K, Kishimoto T, Mimura M, Tsubota K. Sleep and mood disorders in dry eye disease and allied irritating ocular diseases. Sci Rep 2016;6:22480.
32 Sakane Y, Yamaguchi M, Yokoi N, Uchino M, Dogru M, Oishi T,Ohashi Y, Ohashi Y. Development and validation of the Dry Eye-Related Quality-of-Life Score questionnaire. JAMA Ophthalmol 2013;131(10):1331-1338.
33 Αrita R, Itoh K, Inoue K, Αmano S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology 2008;115(5):911-915.
34 Kaido M, Kawashima M, Ishida R, Tsubota K. Relationship of corneal pain sensitivity with dry eye symptoms in dry eye with short tear break-up time. Invest Ophthalmol Vis Sci 2016;57(3):914-919.
35 Niwano Y, Kanno T, Iwasawa Α, Αyaki M, Tsubota K. Blue light injures corneal epithelial cells in the mitotic phase in vitro. Br J Ophthalmol 2014;98(7):990-992.
36 Daral S, Khokhar Α, Pradhan SK. Barriers to disclosure of child maltreatment among school-going adolescent girls of a semi-urban area of Delhi, India. Int J Adolesc Med Health 2016; pii: /j/ijamh.ahead-of-print/ijamh-2016-0014/ijamh-2016-0014.xml.
37 Moriyama M, Kashiwazaki H, Suzuki T. Α secular trend in age at menarche in Japan. Minzoku Eisei 1980;46(1):22-32.
38 Subcommittee of the International Dry Eye WorkShop. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop.Ocul Surf 2007;5(1):75-92.