INTRODUCTION
Peripheral corneal and limbal diseases (PCLD) refer to a series of disorders which affect the peripheral cornea or limbus, including Terrien’s marginal degeneration,Mooren’s ulcer, limbal dermoid, ulcerative keratitis, pellucid marginal corneal degeneration, etc[1-2]. For patients with severe corneal thinning or unhealing ulcers, surgical intervention is necessary. Besides, growing dermoids should be treated with prompt corneal transplantation to prevent amblyopia[3].Peripheral lamellar cornea and limbus transplantation has been proposed for the treatment of PCLD[4-5]. However, the keratolimbal allograft rejection rate is high[6-7]. Moreover,shortages of donor corneas remains a challenge worldwide[8],especially in China[9]. Glycerin cryopreserved limbal lamellar keratoplasty (CLLK) was applied for PCLD[10-12], which could help more patients with limited donor corneas, and decrease the risk of immune rejection by the lowering of the donor’s antigenicity[11-12]. So far, the postoperative recovery process of CLLK has not been demonstrated. Herein, we retrospectively analyzed both the recovery process and the final outcomes of CLLK for PCLD.
SUBJECTS AND METHODS
This study was approved by the Ethics Committee of Wuhan Union Hospital according to the tenets of the Declaration of Helsinki to retrospectively review 12 patients (13 eyes) with PCLD, who underwent CLLK between November 2014 and July 2016.
The donated corneas were obtained from the Red Cross in Wuhan, China. The peripheral corneoscleral rims after lamellar keratoplasty (LK) or penetrating keratoplasty (PK), and those corneas which were not suitable for PK were subjected to microbiological cultures. The donor tissues with negative results were cryopreserved in sterilized pure glycerin (Wuhan Union Hospital) at -20℃ for 7.2±3.4 (ranging from 1 to 12)mo(Table 1).
After local or general anaesthesia, the corneal lesions were removed. The cryopreserved lamellar limbal tissues were pruned to appropriate shape and thickness, and then tightly sutured to the recipient bed with interrupted 10-0 nylon sutures. Concomitant pterygium in one eye was also removed.Tobradex (tobramycin 0.3% and dexamethasone 0.1%, Alcon,FortWorth, TX, USA) eyedrop was administered 4 times per day with weekly tapering, and 1% cyclosporine A (North China Pharmaceutical Co., Ltd.) eyedrop was administered 3 times per day for 6mo. Preservative-free lubricants were used 6 times per day until complete epithelialization. The corneal sutures were removed 1 to 3mo after the surgery. A child with corneal dermoid received amblyopia training after the surgery.All patients were followed up daily until complete graft epithelialization, weekly for 1mo, monthly for 3mo, and then at different intervals after surgery.
Table 1 Patient data and therapeutic outcomes
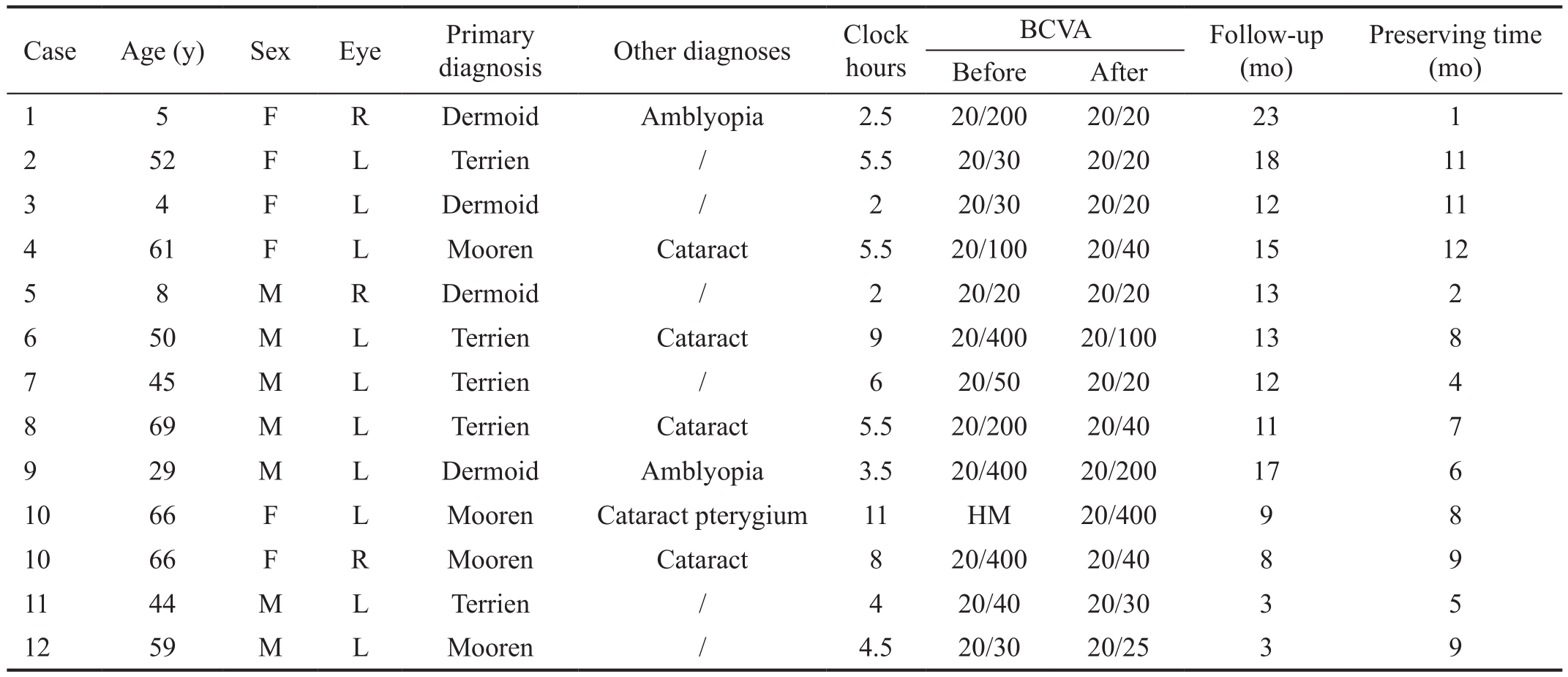
BCVA: Best corrected visual acuity; HM: Hand motion.
RESULTS AND DISCUSSION
Relevant clinical data of each patient are summarized in Table 1. This study included 13 eyes of 12 patients (7 males and 5 females) with a mean age of 41±23.9 (ranging from 4 to 69)y. The mean follow-up was 12.1±5.6 (ranging from 3 to 23)mo. Terrien’s marginal degeneration (Figure 1A1) (5 eyes),Mooren’s ulcer (Figure 1A2) (4 eyes) and corneal dermoid(Figure 1A3) (4 eyes) were enrolled in this study. The mean limbal circumference involvement was 5.3±2.7 (ranging from 2 to 11)h, including less than 4h in 4 eyes, 4-11h in 9 eyes.During the follow-up, neovascularization occurred in 6 eyes(46.2%) at 1mo after surgery but gradually regressed after the continuous use of topical corticosteroids and cyclosporin A.Only 1 patient (7.7%) had corneal ulcer during the followup. The corneal ulcer ultimately healed by the topical use of Tobradex and cyclosporine for 2mo. Eventually, grafts and ocular surface remained stable, and the central corneal stayed smooth and transparent (Figure 1A4, 1A5, 1A6).
The postoperative best corrected visual acuity (BCVA) was improved in 12 eyes and stayed unchanged in 1 eye with normal visual acuity before the surgery (case 5). The BCVA of one child (case 1) with dermoid recovered to 20/20 from 20/200 followed by 22-month amblyopia training after surgery.The duration for graft epithelialization of all 13 eyes varied from 2 to 7d. Epithelialization were from the surrounding recipient limbus in 4 patients (30.8%) with dermoids (Figure 1B1). These patients had less than 4h limbal involvement.The grafts were epithelialized from the surrounding recipient limbus, determined by the arc-shaped fluorescent staining area (Figure 1B2). The epithelialization completed on the postsurgical day 2 (Figure 1B3).
Epithelialization originating from both recipient and graft were observed in 9 eyes (69.2%) with more than or equal to 4h limbal involvement. A 59-year-old patient (case 12)had suffered from Mooren’s ulcer for 5mo (Figure 1C1),which circumferentially involved 4.5h of the limbus (Figure 1C2). The peripheral cornea and limbus were restored after CLLK (Figure 1C3). At postsurgical day 1, the whole graft was stained with fluorescence (Figure 1C4). Two kinds of epithelialization processes were observed at postsurgical day 2 (Figure 1C5). One was from the surrounding recipient(Figure 1C5) and the other was from the graft indicated by a narrow unstained area on the graft limbus (Figure 1C5). The epithelialization completed on day 3 (Figure 1C6).
A 66-year-old woman suffered from Mooren’s ulcer for 3y in both eyes (case 10) was also enrolled. Ocular surface was fully restored and good vision was achieved in her right eye after CLLK (Figure 1A5). There was a pterygium at the nasal region of her left eye (Figure 1D1), besides a crescent shaped ulcer of 11h limbal involvement (Figure 1D1). After perilimbal lamellar keratectomy of the lesion and removal of the pterygium, a lamellar limbus was transplanted (Figure 1D2). The whole cornea stained positive with fluorescein at postoperative day 1 (Figure 1D3). The whole graft stained negative at day 7 (Figure 1D4). The epithelialization of the remaining recipient cornea originated from the autologous nasal limbus (Figure 1D4, 1D5). Epithelial cells covered about one half of the remaining cornea at day 14 (Figure 1D5).A stable ocular surface was eventually achieved 2mo after surgery with negative fluorescent staining (Figure 1D6).
In this study, we discovered that cryopreserved limbal grafts could not only provide a normal limbal structure, but also maintain a stable ocular surface by providing epithelialization sources. It indicates limbal stem cells, which reside deep in the palisade of Vogt[13], may survive in the cryopreserved tissue. It also explains the phenomenon that cornea was fully epithelialized after 360 degree ring-shape CLLK[10]. In the 4 patients with less than 4h limbal involvement, epithelialization were observed only from the surrounding recipient limbus.This may be due to the rapid completion of epithelialization before limbal activation in grafts.
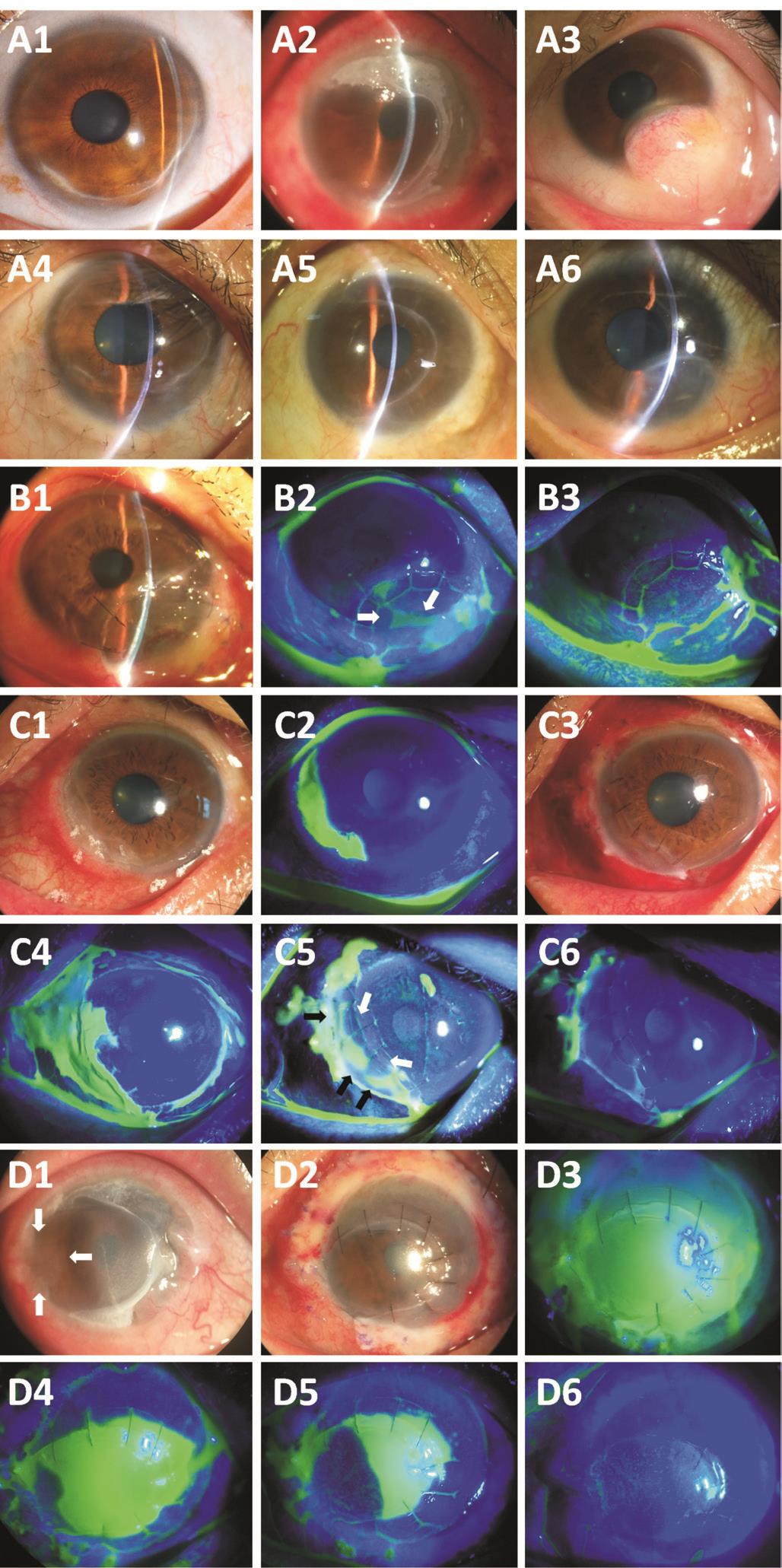
Figure 1 Typical cases A: A patient (case 2) had Terrien’s marginal degeneration (A1). The corneal graft is clear at the postoperative 17mo visit (A4). A patient (case 10 R) suffered from Mooren’s ulcer(A2). The graft remained stable during the 8mo follow-up (A5). A 29-year-old male (case 9) was diagnosed with dermoid (A3). After a round-shaped CLLK, a normal corneal appearance was achieved at the 17mo follow-up (A6). B: At day 1 (B1), the round graft was epithelialized from the recipient limbus, judged by the arc-shaped fluorescent staining (B2, white arrows) and the epithelialization completed at day 2 (B3). C: A patient (case 12) had Mooren’s ulcer(C1, C2). At postsurgical day 1 (C3), the whole graft was stained with fluorescence (C4). Two kinds of epithelialization were recorded at day 2 (C5, white arrows and black arrows). The epithelialization completed at day 3 (C6). D: A 66-year-old woman with Mooren’s ulcer (case 10 L) had a pterygium at her left eye (D1, white arrows).The cornea was reconstructed by CLLK (D2). The whole cornea was positive with fluorescent staining at day 1 (D3). The graft staining was negative at day 7 (D4). The epithelialization of recipient remaining cornea originated from the autologous nasal limbus (D4, D5). A stable ocular surface was eventually achieved at 2mo (D6).
Rejection is considered to be the main failure factor responsible for allogeneic keratoplasty[14]especially in limbal transplantation for the existence of immune cells and vascular tissues[6]. Glycerin cryopreservation promoted graft survival in high-risk cornea transplantation by eliminating most of the cells including keratocytes and bone marrow-derived cells[15].No episode of graft rejection was observed over long-term follow-up after CLLK[11-12]. In our study, only minor degree of immune-rejection in the first month visit was noted and no graft failure happened.
Due to the scarcity of human corneal donors and eye bank services in developing countries, a huge gap presents between the need and supply of donor corneas[8-9]. The advantage of CLLK is that a donor cornea can be fully used, and more patients could benefit from this method.
In conclusion, CLLK is an effective and feasible surgery for PCLD. Cryopreserved limbal grafts can provide epithelialization sources in ocular surface reconstruction.
ACKNOWLEDGEMENTS
Foundations:Supported by National Natural Science Foundation of China (No.81300736; No.81370993).
Conflicts of Interest:Xie HT, None; Li J, None; Liu Y,None; Jiang DL, None; Shen RF, None; Zhang MC, None.
REFERENCES
1 Knox Cartwright NE, Tole DM, Georgoudis P, Cook SD. Peripheral ulcerative keratitis and corneal melt: a 10-year single center review with historical comparison. Cornea 2014;33(1):27-31.
2 Lenk J, Haustein M, Terai N, Spoerl E, Raiskup F. Characterization of ocular biomechanics in pellucid marginal degeneration. Cornea 2016;35(4):506-509.
3 Pirouzian A. Management of pediatric corneal limbal dermoids. Clin Ophthalmol 2013;7:607-614.
4 Cheng CL, Theng JT, Tan DT. Compressive C-shaped lamellar keratoplasty: a surgical alternative for the management of severe astigmatism from peripheral corneal degeneration. Ophthalmology 2005;112(3):425-430.
5 Wang T, Shi W, Ding G, Li S, Liu M, Gao H. Ring-shaped corneoscleral lamellar keratoplasty guided by high-definition optical coherence tomography and Scheimpflug imaging for severe Terrien's marginal corneal degeneration. Graefes Arch Clin Exp Ophthalmol 2012;250(12):1795-1801.
6 Maruyama-Hosoi F, Shimazaki J, Shimmura S, Tsubota K. Changes observed in keratolimbal allograft. Cornea 2006;25(4):377-382.
7 Cheung AY, Holland EJ. Keratolimbal allograft. Curr Opin Ophthalmol 2017;28(4):377-381.8 Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, Thuret G. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol 2016;134(2):167-173.
9 Shang X, Zhang M. Body and organ donation in Wuhan, China. Lancet 2010;376(9746):1033-1034.
10 Bi YL, Bock F, Zhou Q, Cursiefen C. Central corneal epithelium self-healing after ring-shaped glycerin-cryopreserved lamellar keratoplasty in Terrien marginal degeneration. Int J Ophthalmol 2013;6(2):251-252.
11 Gao H, Wang X, Echegaray JJ, Li S, Wang T, Shi W. Partial lamellar keratoplasty for peripheral corneal disease using a graft from the glycerin-preserved corneoscleral rim. Graefes Arch Clin Exp Ophthalmol 2014;252(6):963-968.
12 Huang D, Qiu WY, Zhang B, Wang BH, Yao YF. Peripheral deep anterior lamellar keratoplasty using a cryopreserved donor cornea for Terrien's marginal degeneration. J Zhejiang Univ Sci B 2014;15(12):1055-1063.
13 Lavker RM, Tseng SC, Sun TT. Corneal epithelial stem cells at the limbus: looking at some old problems from a new angle. Exp Eye Res 2004;78(3):433-446.
14 Sellami D, Abid S, Bouaouaja G, Ben Amor S, Kammoun B,Masmoudi M, Dabbeche K, Boumoud H, Ben Zina Z, Feki J.Epidemiology and risk factors for corneal graft rejection. Transplant Proc 2007;39(8):2609-2611.
15 Li J, Yu L, Deng Z, Wang L, Sun L, Ma H, Chen W. Deep anterior lamellar keratoplasty using acellular corneal tissue for prevention of allograft rejection in high-risk corneas. Am J Ophthalmol 2011;152(5):762-770.e3.