A review of combined phacoemulsification and endoscopic cyclophotocoagulation: efficacy and safety
Wen Sun, Chen-Ying Yu, Jian-Ping Tong
Department of Ophthalmology, the First Affiliated Hospital,College of Medicine, Zhejiang University, Hangzhou 310003,Zhejiang Province, China
INTRODUCTION
Glaucoma is characterized by progressive optic nerve damage, often associated with increased intraocular pressure (IOP). Glaucoma has become the leading cause of global irreversible blindness, and it has been estimated that the global prevalence of glaucoma for population aged 40-80y is 3.54%[1]. Up until now, the only treatment strategy proven effective for glaucoma still focuses on the reduction of IOP as always, and this goal could be accomplished either by medication or surgery. Although traditional procedure such as trabeculectomy has been a great success in the history of glaucoma surgery, it is associated with some severe complications and could cause significant structural changes in ocular tissue[2]. With the development of minimally invasive surgical techniques, ophthalmologists began to have a wider range of options in glaucoma treatment, and endoscopic cyclophotocoagulation (ECP) is one of them.
Since the first clinical application by Uram et al[3]in 1992,ECP, as a versatile “minimally invasive glaucoma surgery”(MIGS) procedure, has begun to gain attentions in recent years.ECP could decrease aqueous humor production through ciliary body destruction in a controlled and predictable fashion, and could be regarded as an improved pattern of transscleral ciliary body ablation with direct visualization of the operation site[4].Although ECP was initially performed in refractory glaucoma cases, this procedure could actually be utilized in severe,moderate, or even mild stages of many types of glaucoma[5].
Studies have shown that about one-third of the patients who received glaucoma surgery present with a certain degree of cataract[6]. On the one hand, topical anti-glaucoma medications,laser treatment, and filtering surgery could all accelerate the progression of cataract; On the other hand, cataract may also affect glaucoma patients in the following ways: 1) decreased visual acuity; 2) possible angle closure induced by intumescent cataract; 3) difficulty in evaluation of optic disc and retinal nerve fiber layer; 4) compromised accuracy of visual field examination. As a result, timely extraction of cataract in patients with glaucoma is beneficial for visual improvement and glaucoma management, and it is reasonable to combine phacoemulsification with ECP (Phaco-ECP) as a treatment option for these patients. Recent studies have evaluated the efficacy and safety of Phaco-ECP procedure, but most of them consist of retrospective case series that lack a control group.Therefore, this article intends to review these study reports and provide an evidence-based conclusion for this new treatment strategy.
History and Method of Phaco-endoscopic Cyclophotocoagulation ProcedureThe method of ciliary body destruction as a treatment for glaucoma was first established as early as 1930s, and various means had been used to achieve this goal,such as diathermy, cryotherapy, and even surgical excision[7].With the introduction of ophthalmic laser in the 1970s, transscleral cyclophotocoagulation (TCP) began to come into view.Despite its good tolerance and efficacy, TCP is associated with some serious complications including vision loss, hypotony,and phthisis, so it has mainly been used as a last-resort treatment for intractable glaucoma with very limited visual potential, and repeated treatment is often required[8].
To better control the extent and effect of cyclophotocoagulation treatment, intraocular endoscope was introduced to deliver laser energy in a precise and efficient manner more recently.Studies have shown that the IOP reduction amplitude of ECP was similar or slightly superior to that of TCP, but in terms of the improvement of best-corrected visual acuity (BCVA),ECP gave significantly better results than TCP; Besides,the incidence of serious complications associated with ECP such as hypotony and phthisis was extremely low due to its precise targeting and relatively low level of laser energy[9-10].Moreover, when compared with Ahmed drainage implant in refractory glaucoma, ECP showed excellent results in IOP control with low complication rate[11].
Up until now, phacoemulsification combined with trabeculectomy(Phaco-Trab) still remained the standard therapeutic strategy for the management of coexisting glaucoma and cataract[12].But patients treated with Phaco-Trab procedure will need a longer period of recovery, during which some early complications of filtering surgery may occur such as wound leakage and hypotony, shallow or flat anterior chamber, and serous or hemorrhagic ciliochoroidal effusions[13]. Its late complications may include bleb-related endophthalmitis, bleb leakage or failure, and ocular hypotony or even phthisis. In order to closely monitor the surgical outcomes of Phaco-Trab and handle these disturbing problems in time, repeated followups may be necessary[14]. In contrast, a variety of studies have confirmed the efficacy and safety profile of ECP, and although the procedure was originally used in refractory and pediatric glaucoma[9,11,15-17]. Researchers have noted that for patients with coexisting cataract and glaucoma, ECP could be applied at an earlier stage of disease[18]. Moreover, since ECP could be performed through the same corneal incision,many ophthalmologists have chosen ECP as an adjunct to phacoemulsification, creating this new combining procedure called “Phaco-ECP”[19]. Therefore, with the development of ECP, Phaco-ECP gradually became a well-accepted surgical option, sparing patients the adverse effects of traditional filtering surgery while preserving the advantages of minimally invasive cataract surgery.
Phaco-ECP is usually performed through the following steps:1) phacoemulsification is first performed via a 2.0-3.0 mm clear corneal incision under peri- or retrobulbar anesthesia; 2)viscoelastic is injected beneath the iris to expand the ciliary sulcus; 3) the ECP probe available in 19, 20, or 23 gauge size,which contains a diode laser (wavelength of 810 nm), a xenon light source (175 W), a helium-neon aiming beam, and most important of all an endoscope, is then inserted into the anterior chamber via the clear corneal incision[3]; 4) laser energy and exposure duration could be set according to the treatment requirements and surgeons’ experiences, and these parameters could be adjusted while observing the reaction of ciliary process to make sure the photocoagulation is sufficient for cyclodestruction; 5) for a more significant IOP lowering effect,another or more clear corneal incisions could be made to cover a wider scope of ciliary process[20-21]. Corneal incisions made during the procedure could be routinely left unsutured. About intraocular lens (IOL) insertion, most researchers would insert the IOL into the capsular bag after cyclophotocoagulation[3],but Chen et al[22]asserted that IOL insertion beforehand would help protect the posterior capsule.
Histopathology of Endoscopic Cyclophotocoagulation ProcedureBoth ECP and TCP focus on ciliary process ablation to achieve aqueous suppression, but the energy level of ECP could be titrated during procedure to maximize its effect while avoiding overtreatment, therefore a clear distinction exists between ECP and TCP when evaluating the extent of tissue destruction.
In 2007, Pantcheva et al[23-24]from University of Pittsburgh studied the acute histological effects of TCP and ECP on the ciliary body and other ocular structures in porcine and human eyes. They found that tissues treated with TCP exhibited pronounced tissue disruption of the ciliary body muscle and stroma, ciliary processes, and both pigmented and nonpigmented ciliary epithelium. In contrast, tissues treated with ECP exhibited less architectural disorganization and sparing of the ciliary body muscle, although pronounced contraction of the ciliary processes with disruption of the ciliary body epithelium could be observed. However, the sclera was not affected by either laser treatment. These results were also supported by reports from other researchers[25-26], leading to the conclusion that ECP seems to be a more selective form of cyclophotocoagulation that results in less tissue disruption while achieving the goal of destroying ciliary body epithelium.Besides the direct destruction of the ciliary epithelium by laser ablation, vascular changes are responsible for the decrease of IOP as well. Schlote et al[27]examined the vascular casts of ciliary body in rabbit eyes after TCP treatment and observed a marked rarefication of capillary network within the treated areas of ciliary body at all follow-ups. On the other hand, Lin et al[28]also used a rabbit model to compare the vascular effects of ECP versus TCP, and they found that the ciliary processes showed some reperfusion at 1wk and greater reperfusion by 1mo after ECP treatment, but no reperfusion was shown after TCP treatment. These results can be partly the reason why ECP,unlike TCP, is less associated with significant complications of cyclodestruction including hypotony and phthisis.
Clinical Indications of Phaco-endoscopic Cyclophotocoagulation ProcedureAlthough there was no set standard for the indication of Phaco-ECP, the procedure was usually performedin glaucoma patients with visually significant cataract, and the glaucoma conditions may include: 1) medically uncontrolled glaucoma; 2) previously failed IOP-lowering surgery such as trabeculectomy, glaucoma drainage device or TCP; 3) refractory glaucoma such as pseudoexfoliation or rubeotic glaucoma[29].After comparing ECP with trabeculectomy, Berke et al[30]noted that easier procedure technique of ECP guaranteed its shorter operation time, and ECP was more suitable in patients who may present difficulty in drainage channel formation during filtering surgery (including conditions such as elevated venous pressure of superficial scleral vein, intraocular tumor, and blepharitis), while less associated with repeated postoperative follow-ups and additional treatment (including laser loosening of scleral flap suture, filtering bleb puncture, and subconjunctival injection of 5-FU). As a result, they suggested that Phaco-ECP could be used in any patient who may need combined glaucoma and cataract surgery. And for patients who anticipate a future filtering surgery, Phaco-ECP could serve as an initial step for temporary control of IOP until the ocular surface condition has improved enough to allow surgery. Furthermore, for patients with complex secondary glaucoma where the use of traditional incisional surgery and other MIGS procedures are all contraindicated as in scleromalacia, ECP can be safely and successfully used to control IOP[31]. However, since ECP procedure is destructive in its own nature no matter how mild the damage might be, it could not be an equivalent substitute for filtration surgery in all glaucoma patients, and more large-scale and comprehensively designed clinical trials should be carried out before officially expanding its indications.
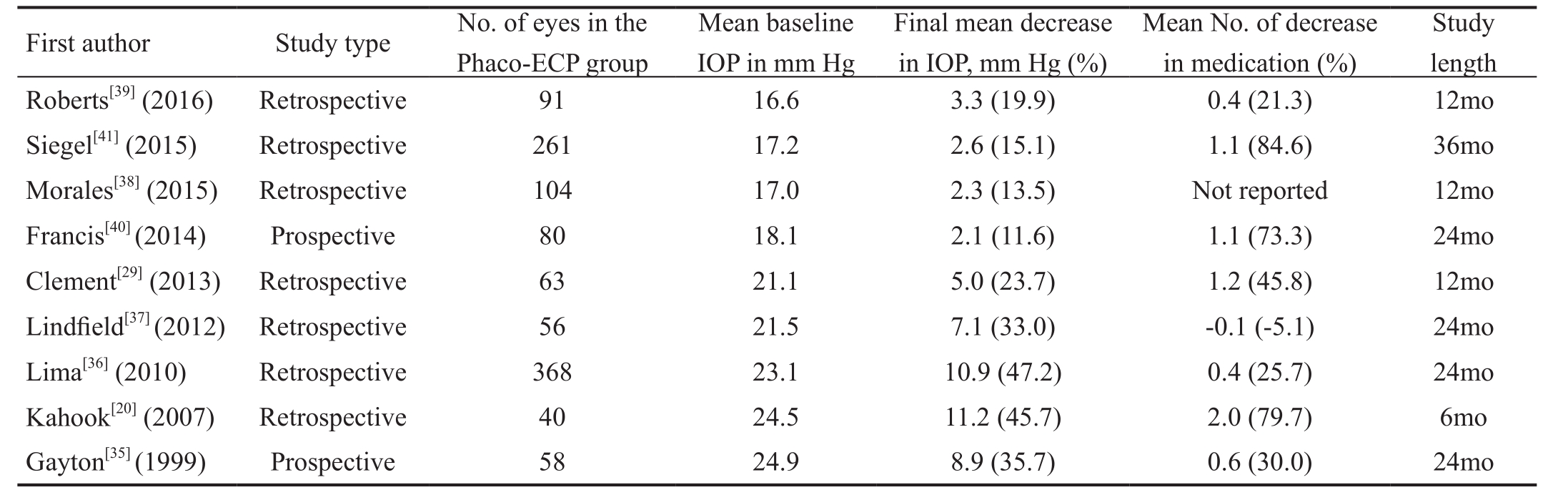
Table 1 Review of published results for Phaco-ECP
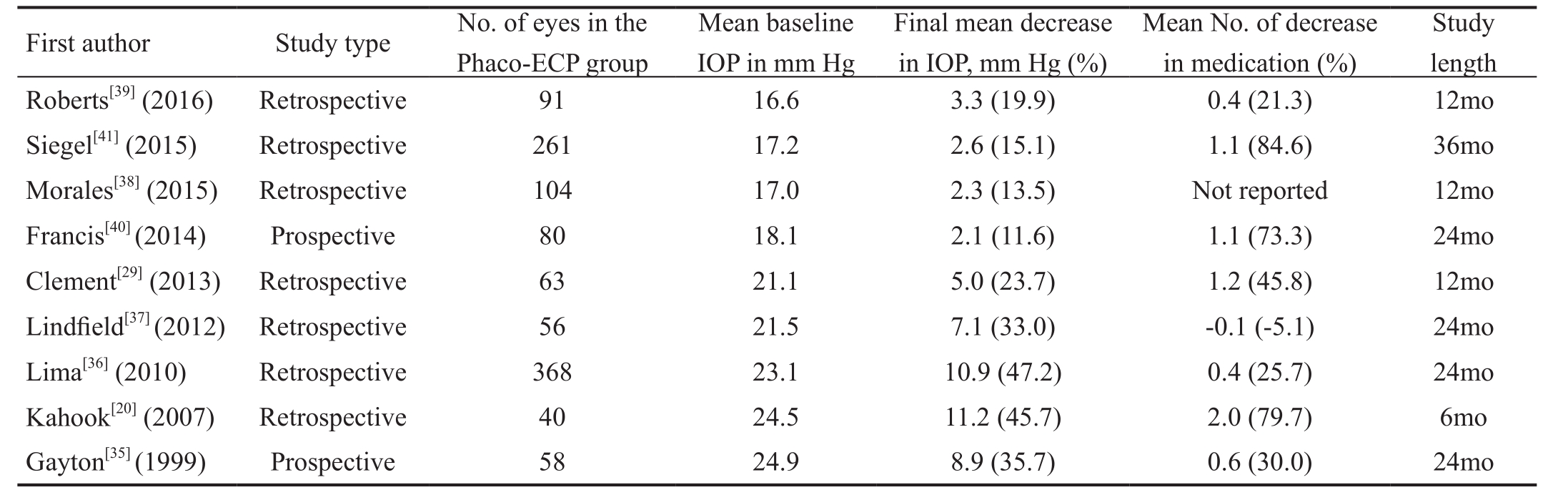
ECP: Endoscopic cyclophotocoagulation.
Study length Roberts[39](2016) Retrospective 91 16.6 3.3 (19.9) 0.4 (21.3) 12mo Siegel[41](2015) Retrospective 261 17.2 2.6 (15.1) 1.1 (84.6) 36mo Morales[38](2015) Retrospective 104 17.0 2.3 (13.5) Not reported 12mo Francis[40](2014) Prospective 80 18.1 2.1 (11.6) 1.1 (73.3) 24mo Clement[29](2013) Retrospective 63 21.1 5.0 (23.7) 1.2 (45.8) 12mo Lindfield[37](2012) Retrospective 56 21.5 7.1 (33.0) -0.1 (-5.1) 24mo Lima[36](2010) Retrospective 368 23.1 10.9 (47.2) 0.4 (25.7) 24mo Kahook[20](2007) Retrospective 40 24.5 11.2 (45.7) 2.0 (79.7) 6mo Gayton[35](1999) Prospective 58 24.9 8.9 (35.7) 0.6 (30.0) 24mo First author Study type No. of eyes in the Phaco-ECP group Mean baseline IOP in mm Hg Final mean decrease in IOP, mm Hg (%)Mean No. of decrease in medication (%)
Clinical Outcomes of Phaco-endoscopic Cyclophotocoagulation ProcedureGiven the fact that cataract and glaucoma frequently coexist in elderly patients, and that ECP can be easily performed through a clear corneal incision used for cataract phacoemulsification, Phaco-ECP procedure began to emerge recently as a new option for combined cataract and glaucoma surgery. We searched PubMed/MEDLINE using the terms“endoscopic cyclophotocoagulation” and “phacoemulsification” combined to look for relative studies and found a few studies in the last few years showing encouraging results with this procedure (Table 1).
EfficacyIn 1995, Uram et al[32], who first realized the clinical application of ECP, made a prospective evaluation about the efficacy and safety of Phaco-ECP in ten patients with refractory open angle glaucoma and cataract. The results were quite impressive, showing a significant decrease of mean IOP. However, at that time, Phaco-Trab had already been well documented to be effective in the treatment of coexisting glaucoma and cataract[33-34], and due to the lack of equipment, ECP was not extensively carried out. In 1999,Gayton et al[35]compared patients receiving Phaco-Trab with those receiving Phaco-ECP to assess the differences in efficacy and complications after the two procedures. This randomized prospective study revealed that after a mean follow-up of 2y, 30% of Phaco-ECP patients achieved IOP control (below 19 mm Hg) without medication and 65% with medication,while 40% of Phaco-Trab patients achieved control without medication and 52% with medication. Besides, additional surgical intervention was required in 14% of Phaco-ECP patients and 10% of Phaco-Trab patients. Based on the results of comparison, Gayton et al[35]concluded that Phaco-ECP was a reasonably safe and effective alternative to Phaco-Trab.
Considering the complications related to trabeculectomy, such as infection, hypotony, and leakage or failure of the filtering bleb,Phaco-ECP was gradually accepted by more ophthalmologists with the development of MIGS. But most studies reporting the outcomes of Phaco-ECP are retrospective case series that lack a control group. Lima et al[36]from Brazil evaluated 368 eyes from 243 patients with primary open angle glaucoma(POAG) and cataract. They discovered that the postoperative IOP (average value around 11-13 mm Hg) was significantly lower than the preoperative IOP (23.07±5.52 mm Hg) at all follow-ups (1d, 1, 6, 12 and 24mo), and as a result, the number of IOP-lowering medications taken by these patients also decreased (from 1.44±0.97 agents pre-op to 0.37±0.68 agents 24mo post-op). Similar result regarding IOP-lowering effects of Phaco-ECP was reported by Lindfield et al[37]as well. They observed a mean IOP drop of 7.1 mm Hg from baseline to 18 and 24mo post-op, and statistically significant decrease in IOP was demonstrated at all-time points. However, in their study,the mean medication usage was 1.97 agents at baseline, 1.96 agents at 18mo and 2.07 agents at 24mo with no statistically significant change throughout. Clement et al[29], Morales et al[38]and Roberts et al[39]each performed a retrospective study assessing the efficacy of Phaco-ECP procedure with about one-year follow-up. The studies all demonstrated good IOP lowering efficacy as well as a reduction in medication burden after Phaco-ECP treatment. At the same time, Morales et al[38]noted that eyes with POAG had higher success rate compared with primary angle-closure and pseudoexfoliation glaucoma,while Roberts et al[39]suggested the only predictive factor for success was a higher preoperative IOP. Besides, with the removal of cataract, the mean BCVA was significantly improved in all five studies mentioned above.
More recently, to further clarify the efficacy of Phaco-ECP,randomized clinical trials comparing phacoemulsification alone with Phaco-ECP were conducted by several researchers.Francis et al[40]reported that in the Phaco-ECP group, the mean IOP decreased from 18.1±3.0 mm Hg pre-op to 16.0±3.3 mm Hg 2-year post-op, and the number of IOP-lowering medication decreased from 1.5±0.8 pre-op to 0.4±0.7 2-year post-op. In contrast, during the same follow-up period, the mean IOP and the number of IOP-lowering medication in the Phaco group remained almost unchanged; And the difference in IOP and medication reduction between the 2 groups was statistically significant at all-time points. Differed from Francis, Siegel et al[41]reported that there was not a statistically significant difference between Phaco-ECP and Phaco group in their IOP lowering efficacy at any post-operative visit; However they discovered that mean medication reliance in the Phaco-ECP group was only 0.2±0.6 agents while that in the Phaco group was 1.3±0.6 agents at 36-month post-op; And the full success rate (defined as minimum 20% IOP reduction with a decrease of at least one ocular hypertensive medication) in the Phaco-ECP group was significantly higher than that in the Phaco group (61.4% versus 23.3%).
Phaco-ECP procedure also has been carried out in Asian countries, but the number of published studies was relatively smaller than that from western countries. In 2009, Yip et al[42]found that ECP may have a treatment role in Asian patients with glaucoma, but the success rate appeared poorer than previously reported in Caucasian populations, and the treatment effect appeared to wane between 18 and 24mo post-treatment.The other two studies[43-44]performed in Chinese population showed excellent results regarding the efficacy and safety of Phaco-ECP. In these studies, mean post-treatment IOP was significantly lowered with decreased number of antiglaucoma medications and improved visual acuity. As a result,researchers have concluded that Phaco-ECP was not only effective and safe in the treatment of uncontrolled late stage glaucoma combined with cataract[43], but also could be used as one of the first choice operation for glaucoma and cataract patients[44].
SafetyThe less invasive nature of ECP has enabled it to avoid some serious complications associated with traditional filtering surgery, and its lacking of implants is also an obvious advantage over other MIGS, sparing it the possible implantrelated complications. Complications associated with ECP in the ECP Collaborative Study were as follows: IOP spike(14.5%), hemorrhage (3.8%), serous choroidal effusion(0.36%), retinal detachment (0.27%), and hypotony or phthisis(0.12%), etc. No chronic inflammation or endophthalmitis was observed, and the incidence of serious complications was very low and occurred primarily in refractory glaucoma patients[8].When Phaco and ECP are combined into one procedure, its postoperative complications are actually similar to those of ECP alone. Lima et al[36]reported the complications included immediate postoperative IOP spike (14.4%), postoperative fibrin exudates in anterior chamber (7.06%), cystoid macular edema (4.34%), transitory hypotony (2.17%), and iris bombe(1.08%). Furthermore, intraoperative complications reported by Morales et al[38]included posterior capsular rupture with vitreous loss (3.85%), Descemet’s membrane detachment(1.92%), and zonular dialysis (0.96%).
IOP spikes seems to be the most common postoperative complication of Phaco-ECP after reviewing all these articles,and it was usually attributed to transient inflammation in the anterior chamber immediately after procedure, or sometimes due to retained viscoelastic. These IOP spikes could be treated by temporarily increasing IOP-lowering medications and/or steroid drop frequency at the discretion of the surgeon,and generally speaking, the condition would have resolved by one month post-op. A fibrinous reaction in the anterior chamber secondary to inflammatory reaction caused by ECP was also common, and in some cases fibrinous uveitis would develop. This complication could be treated with intensive topical steroid therapy with resolution time ranged from 4 to 10wk[29], and intracameral dexamethasone injection at the end of procedure might be a preventive measure to the problem.Overall, serious complications such as retinal detachment,intraocular hemorrhage requiring surgical intervention,choroidal hemorrhage, chronic uveitis, IOL dislocation,endophthalmitis, and hypotony were rare with Phaco-ECP procedure, and adding ECP did not increase the risk for serious complications compared with Phaco alone[40]. However, since the pressure-lowering effect of cyclodestruction cannot be reversed, persistent hypotony and phthisis are most concerning.
Theoretically, the incidence of hypotony should be lower with a smaller treatment area, but this has not been formally analyzed, and no linear correlation has been established yet.With more experience in performing the procedure, less hypotony cases were seen after Phaco-ECP. According to one recent study performed by Marco et al[45], none of the patients suffered from postoperative hypotony in the Phaco-ECP group,while five patients from the Phaco-Trab group developed hypotony within the 1stweek post-op although their IOPs all returned normal by the 1stmonth visit.
Since cataract surgery could be considered as a refractive surgery in a sense, it is essential to have the actual postoperative refractive outcome same as the preoperative predicted value.As the lens zonules are attached to the ciliary body, change in ciliary body position after ECP may induce a change in the effective lens position, which may bring in unwanted refractive error and decrease postoperative visual quality. A newly reported trial conducted by Sheybani et al[46]addressed this issue, and revealed that the Phaco-ECP group had significantly more myopic postoperative refractive outcomes, and more variability in refractive outcomes when compared with standard cataract surgery. Similar results were also obtained by Wang et al[47]in angle-closure eyes, suggesting a small myopic shift after Phaco-ECP procedure. However, Kang et al[48]discovered that more than 90% of eyes in Phaco-ECP group achieved post-operative refraction within ±1 diopter of the target refraction, which showed no significant difference when compared to phacoemulsification alone. These results can serve as a reminder for surgeons to make appropriate adjustment to lens power selection before performing Phaco-ECP procedure.
LimitationsSeveral limitations existed when we reviewed these clinical trials mentioned above. 1) Most of the clinical data came from Caucasian population, and there was a relative lack of data indicating the efficacy of Phaco-ECP in Asian population. Racial differences may affect pigmentation of ocular structures including ciliary epithelium, thus enhancing or compromising the effects of ECP, and it has been noted by Yip et al[42]. Therefore, the efficacy and safety problem of Phaco-ECP procedure should be further evaluated in Asian population; 2) Patients with POAG were not separated from patients diagnosed with other types of glaucoma when being evaluated, which may become a confounding factor since POAG patients may respond better to Phaco-ECP procedure[38]while serious complications may be more prone to occur in secondary glaucoma patients; 3) The laser power level and treatment extent adopted in each clinical trial differed from one another, therefore it remained to be determined how much IOP-lowering effects could be generated by a certain extent of ECP treatment in different types of glaucoma. Animal studies have been performed to seek the appropriate laser energy level to effectively treat the ciliary epithelium[49-50];
However, no such study could be found regarding the “energyeffect” evaluation of Phaco-ECP procedure in human eyes.As to the treatment extent, a single clear cornea incision allows approximately 240 to 300 degrees of treatment, and the remaining 60 to 120 degrees of ciliary processes under the corneal incision are often left untreated. As a result, more than one corneal incision may be necessary to ablate the rest of the ciliary processes. Kahook et al[20]conducted a study to compare the IOP-lowering effect of Phaco-ECP treatment through one versus two corneal incisions. The study revealed that two-site Phaco-ECP may result in statistically significant IOP lowering and less dependence on glaucoma medications compared with single site Phaco-ECP, indicating the influences that treatment extent may have on the efficacy of Phaco-ECP procedure. An animal study conducted by Zhang et al[21]concluded that a treatment extent of about 180 to 270 degrees would be better for IOP control, but the exact parameter used for human eyes remains to be further clarified by future studies; 4) All the studies reviewed in this article had follow-ups no longer than 36mo. Regarding the reperfusion of ciliary processes after ECP treatment[28], its IOP-lowering effect may be weakened in the long run, so longer follow-up period may be needed to observe the long-term efficacy of Phaco-ECP procedure.
Combining cataract and glaucoma surgery, Phaco-ECP emerged as an alternative solution to the coexisting problems with its minimally invasive nature. Up until now, all the studies evaluating the efficacy data pertaining to Phaco-ECP procedure gave promising results, implying that the procedure is effective in IOP control and visual acuity improvement. Besides, the safety profile of Phaco-ECP was also excellent when compared with traditional anti-glaucoma surgery such as trabeculectomy and TCP, rarely showing any serious complications. Since ECP could be performed in a quantitative way and under direct visualization, it could spare patients the risks of phthisis that might be caused by other destructive procedures. However, due to its relatively short period of application and lack of largescale multicenter clinical study, more data is needed to clarify its long-term efficacy and the association between treatment extent and IOP lowering effect before introducing Phaco-ECP as a routine therapeutic option for patients with moderate or even early glaucoma.
ACKNOWLEDGEMENTS
Foundation:Supported by the Science and Technology Foundation of Zhejiang Province, China (No.2015C33191).
Conflicts of Interest:Sun W, None; Yu CY, None; Tong JP,None.
REFERENCES
1 Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY.Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014;121(11):2081-2090.
2 Gedde SJ, Herndon LW, Brandt JD, Budenz DL, Feuer WJ,Schiffman JC; Tube Versus Trabeculectomy Study Group. Postoperative complications in the Tube Versus Trabeculectomy (TVT) Study during five years of follow-up. Am J Ophthalmol 2012;153(5):804-814.e1.
3 Uram M. Endoscopic cyclophotocoagulation in glaucoma management.Curr Opin Ophthalmol 1995;6(2):19-29.
4 Francis BA, Kwon J, Fellman R, Noecker R, Samuelson T, Uram M,Jampel H. Endoscopic ophthalmic surgery of the anterior segment. Surv Ophthalmol 2014;59(2):217-231.
5 Seibold LK, SooHoo JR, Kahook MY. Endoscopic cyclophotocoagulation.Middle East Afr J Ophthalmol 2015;22(1):18-24.
6 Uram M. Endoscopic surgery in ophthalmology. Lippincott: Williams &Wilkins, 2003;110.
7 Allingham RR, Damji KF, Shields MB. Shields Textbook of Glaucoma.Vol. 14, 6th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins, 2011; 610.
8 Ishida K. Update on results and complications of cyclophotocoagulation.Curr Opin Ophthalmol 2013;24(2):102-110.
9 Lin S. Endoscopic cyclophotocoagulation. Br J Ophthalmol 2002;86(12):1434-1438.
10 Neely DE, Plager DA. Endocyclophotocoagulation for management of difficult pediatric glaucomas. J AAPOS 2001;5(4):221-229.
11 Lima FE, Magacho L, Carvalho DM, Susanna R Jr, Avila MP. A prospective, comparative study between endoscopic cyclophotocoagulation and the Ahmed drainage implant in refractory glaucoma. J Glaucoma 2004;13(3): 233-237.
12 Goh ES, Lim BA, Yip L. Endoscopic cyclophotocoagulation: an overview and Asian perspective. Ann Acad Med Singapore 2007;36(Suppl):50-55.
13 Teekhasaenee C, Ritch R. Combined phacoemulsification and goniosynechialysis for uncontrolled chronic angle-closure glaucoma after acute angle-closure glaucoma. Ophthalmology 1999;106(4):669-674.
14 Tanihara H, Nagata M. Complications of goniosynechialysis. Special reference to fibrin-like exudate. Nippon Ganka Gakkai Zasshi 1988;92(3):444-447.
15 Plager DA, Neely DE. Intermediate-term results of endoscopic diode laser cyclophotocoagulation for pediatric glaucoma. J AAPOS 1999;3(3):131-137.
16 Al-Haddad CE, Freedman SF. Endoscopic laser cyclophotocoagulation in pediatric glaucoma with corneal opacities. J AAPOS 2007;11(1):23-28.17 Carter BC, Plager DA, Neely DE, Sprunger DT, Sondhi N, Roberts GJ. Endoscopic diode laser cyclophotocoagulation in the management of aphakic and pseudophakic glaucoma in children. J AAPOS 2007;11(1):34-40.
18 Lin SC. Endoscopic and transscleral cyclophotocoagulation for the treatment of refractory glaucoma. J Glaucoma 2008;17(3):238-247.
19 Mora JS, Iwach AG, Gaffney MM, Wong PC, Nguyen N, Ma AS,Dickens CJ. Endoscopic diode laser cyclophotocoagulation with a limbal approach. Ophthalmic Surg Lasers 1997;28(2):118-123.
20 Kahook MY, Lathrop KL, Noecker RJ. One-site versus two-site endoscopic cyclophotocoagulation. J Glaucoma 2007;16(6):527-530.
21 Zhang YJ, Yu FL, Huang GF, Liu M. Lowing-IOP effect of endoscopic cyclophotocoagulation combined with phacoemulsification and IOL in rabbit chronic glaucomatous eye. Chin J Exp Ophthalmol 2015;33(3):232-236.
22 Chen J, Cohn RA, Lin SC, Cortes AE, Alvarado JA. Endoscopic photocoagulation of the ciliary body for treatment of refractory glaucomas. Am J Ophthalmol 1997;124(6):787-796.
23 Pantcheva MB, Kahook MY, Schuman JS, Rubin MW, Noecker RJ.Comparison of acute structural and histopathological changes of the porcine ciliary processes after endoscopic cyclophotocoagulation and transscleral cyclophotocoagulation. Clin Exp Ophthalmol 2007;35(3):270-274.
24 Pantcheva MB, Kahook MY, Schuman JS, Noecker RJ. Comparison of acute structural and histopathological changes in human autopsy eyes after endoscopic cyclophotocoagulation and trans-scleral cyclophotocoagulation. Br J Ophthalmol 2007;91(2):248-252.
25 McKelvie PA, Walland MJ. Pathology of cyclodiode laser: a series of nine enucleated eyes. Br J Ophthalmol 2002;86(4):381-386.
26 Lin M, Ge J, Huang S, Yu M, Zheng J. The histopathologic changes of human eyes after laser endoscopic cyclophotocoagulation. Eye Sci 2004;20(4):233-236.
27 Schlote T, Beck J, Rohrbach JM, Funk RH. Alteration of the vascular supply in the rabbit ciliary body by transscleral diode laser cyclophotocoagulation.Graefes Arch Clin Exp Ophthalmol 2001;239(1):53-58.
28 Lin SC, Chen MJ, Lin MS, Howes E, Stamper RL. Vascular effects on ciliary tissue from endoscopic versus trans-scleral cyclophotocoagulation.Br J Ophthalmol 2006;90(4):496-500.
29 Clement CI, Kampougeris G, Ahmed F, Cordeiro MF, Bloom PA.Combining phacoemulsification with endoscopic cyclophotocoagulation to manage cataract and glaucoma. Clin Exp Ophthalmol 2013;41(6):546-551.30 Berke SJ. Combined phacoemulsification and ECP. Cataract Refract Surg Today 2008;7:61-64.
31 As Rodrigues I, Lindfield D, R Stanford M, Goyal S. Glaucoma surgery in scleromalacia: using endoscopic cyclophotocoagulation where conventional filtration surgery or angle procedures are contraindicated. J Curr Glaucoma Pract 2017;11(2):73-75.
32 Uram M. Combined phacoemulsification, endoscopic ciliary process photocoagulation, and intraocular lens implantation in glaucoma management. Ophthalmic Surg 1995;26(4):346-352.
33 Samuelson TW. Management of coincident cataract and glaucoma.Curr Opin Ophthalmol 1993;4(1):90-96.
34 Wedrich A, Menapace R, Radax U, Papapanos P. Long-term results of combined trabeculectomy and small incision cataract surgery. J Cataract Refract Surg 1995;21(1):49-54.
35 Gayton JL, Van Der Karr M, Sanders V. Combined cataract and glaucoma surgery: trabeculectomy versus endoscopic laser cycloablation.J Cataract Refract Surg 1999;25(9):1214-1219.
36 Lima FE, Carvalho DM, Avila MP. Phacoemulsification and endoscopic cyclophotocoagulation as primary surgical procedure in coexisting cataract and glaucoma. Arq Bras Oftalmol 2010;73(5):419-422.
37 Lindfield D, Ritchie RW, Griffiths MF. 'Phaco-ECP': combined endoscopic cyclophotocoagulation and cataract surgery to augment medical control of glaucoma. BMJ Open 2012;2(3). pii: e000578.
38 Morales J, Al Qahtani M, Khandekar R, Al Shahwan S, Al Odhayb S, Al Mobarak F, Edward DP. Intraocular pressure following phacoemulsification and endoscopic cyclophotocoagulation for advanced glaucoma: 1-year outcomes. J Glaucoma 2015;24(6):e157-e162.
39 Roberts SJ, Mulvahill M, SooHoo JR, Pantcheva MB, Kahook MY,Seibold LK. Efficacy of combined cataract extraction and endoscopic cyclophotocoagulation for the reduction of intraocular pressure and medication burden. Int J Ophthalmol 2016;9(5):693-698.
40 Francis BA, Berke SJ, Dustin L, Noecker R. Endoscopic cyclophotocoagulation combined with phacoemulsification versus phacoemulsification alone in medically controlled glaucoma. J Cataract Refract Surg 2014;40(8):1313-1321.
41 Siegel MJ, Boling WS, Faridi OS, Gupta CK, Kim C, Boling RC, Citron ME, Siegel MJ, Siegel LI. Combined endoscopic cyclophotocoagulation and phacoemulsification versus phacoemulsification alone in the treatment of mild to moderate glaucoma. Clin Exp Ophthalmol 2015;43(6):531-539.
42 Yip LW, Yong SO, Earnest A, Ji J, Lim BA. Endoscopic cyclophotocoagulation for the treatment of glaucoma: an Asian experience.Clin Exp Ophthalmol 2009;37(7):692-697.
43 Wang H, Tang X. The preliminary efficacy of cataract phacoemulsification and aspiration combined endoscopic cyclophotocoagulation in patients of glaucoma with cataract. Chin J Ocul Traum Occupat Eye Dis 2013;35(9):641-644.
44 Wang F, Feng X, Wang JT. Phacoemulsification and intraocular lens implantation combined with endoscopiccyclophotocoagulation for glaucoma and cataract. Rec Adv Ophthalmol 2014;34(5):458-461.
45 Marco S, Damji KF, Nazarali S, Rudnisky CJ. Cataract and glaucoma surgery: endoscopic cyclophotocoagulation versus trabeculectomy.Middle East Afr J Ophthalmol 2017;24(4):177-182.
46 Sheybani A, Saboori M, Kim JM, Gammon H, Lee AY, Bhorade AM. Effect of endoscopic cyclophotocoagulation on refractive outcomes when combined with cataract surgery. Can J Ophthalmol 2015;50(3):197-201.
47 Wang JC, Campos-Möller X, Shah M, Sheybani A, Ahmed II. Effect of endocyclophotocoagulation on refractive outcomes in angle-closure eyes after phacoemulsification and posterior chamber intraocular lens implantation. J Cataract Refract Surg 2016;42(1):132-137.
48 Kang S, Luk S, Han H, Cordeiro MF, Ahmed F, Bloom P, Crawley L.Refractive outcome of combined phacoemulsification and endoscopic cyclophotocoagulation. Int Ophthalmol 2017;37(6):1311-1317.
49 Harrington JT, McMullen RJ Jr, Cullen JM, Gilger BC. Evaluation of diode endoscopic cyclophotocoagulation in bovine cadaver eyes. Am J Vet Res 2012;73(9):1445-1452.
50 Harrington JT, McMullen RJ Jr, Cullen JM, Campbell NB, Gilger BC.Diode laser endoscopic cyclophotocoagulation in the normal equine eye.Vet Ophthalmol 2013;16(2):97-110.
Correspondenceto:Jian-Ping Tong. Department of Ophthalmology, the First Affiliated Hospital, College of Medicine,Zhejiang University, No.79, Qingchun Road, Hangzhou 310003, Zhejiang Province, China. 1196041@zju.edu.cn
Received:2018-02-24 Accepted: 2018-05-21
Abstract● As cataract occurs frequently in patients with glaucoma,combining phacoemulsification and endoscopic cyclophotocoagulation has been gaining attention recently due to its minimally invasive nature. A variety of studies had evaluated the efficacy and safety of this procedure and had shown extremely promising results. This review article has shown here that combined phacoemulsification and endoscopic cyclophotocoagulation procedure could effectively reduce intraocular pressure in medically uncontrolled glaucoma patients while avoiding serious complications associated with traditional cyclophotocoagulation procedure and adverse effects related to filtering surgery such as trabeculectomy.
● KEYWORDS:endoscopic cyclophotocoagulation;phacoemulsification; glaucoma
DOl:10.18240/ijo.2018.08.23
Citation:Sun W, Yu CY, Tong JP. A review of combined phacoemulsification and endoscopic cyclophotocoagulation: efficacy and safety. Int J Ophthalmol 2018;11(8):1396-1402