INTRODUCTION
M acular oedema is common complication after phacoemulsification surgery in diabetic patients,even with uncomplicated cases[1]. Macular oedema is one of the main causes of unfavorable visual outcome after cataract surgery. Previous studies reported that incidence of clinical cystoid macular oedema (CMO) after phacoemulsification is up to 2.35%[2]. However, other, reported up to 9% angiographic CMO and increased foveal thickness measured by optical coherence tomography (OCT)[3]. Although, the mechanism of CMO is still controversial, the most acceptable is intraocular
inflammation and prostaglandin release that break the blood
retinal barrier increasing permeability and passage of liquid to subfoveal space[4]. This is the cause of the use of nepafenac in treatment of CMO. Post-operative CMO is more commonly seen in patients with non-insulin dependent diabetes mellitus(NIDDM) than insulin dependent. Macular changes in diabetic patients are accelerated by cataract surgery[5]. Nepafenac is non-steroidal anti-inflammatory drug (NSAIDs) which decrease pro-inflammatory prostaglandin by their inhibitor effect on cyclooxygenase[6]. Nepafenac can penetrate corneal epithelium. Nepafenac is converted to active amfenac within the eye producing its anti-inflammatory effect[7]. Amfenac is a highly potent inhibitor of prostaglandin (PGs) production through inhibition of both Cox-1 and Cox-2, but can’t penetrate the corneal epithelium[8].
The aim of this study was to evaluate the effectiveness of nepafenac in prevention of CMO after phacoemulsification in diabetic patients, and to evaluate its toxicity on the retina.
SUBJECTS AND METHODS
Ethical Approval All subjects were carried out in accordance with the tenets of the Declaration of Helsinki (1989) of the World Medical Association. The study was approved by Mansoura International Review Board Ethics Committee. Each patient signed a written consent.
The study was done randomized. This study was carried out on patients attending the Out Patient Clinic of Mansoura Ophthalmic Center during the period from May 2015 to December 2017. The study included 100 eyes of 100 diabetic patients with senile cataract. They were divided into two groups. Group 1 included 50 eyes of 50 patients received perioperative nepafenac 0.1% and Group 2 included also 50 eyes of 50 patients (control group).
Inclusion Criteria Diabetic patients (without diabetic fundal changes) with senile immature cataract underwent phacoemulsification with posterior chamber intraocular lens(PC-IOL).
Exclusion Criteria Ten patients were excluded from the study. Any anterior segment pathology: as corneal opacities,pseudoexfoliation syndrome or dense cataract interfering with OCT imaging or multifocal electroretinogram (MFERG) fixation. Any posterior segment pathology: as, diabetic retinopathy (DR) previous retinal photocoagulation therapy,diabetic macular edema, history of uveitis.
Any intraoperative or post-operative complications. Any medication may interfere with the assessment of the study outcome measures. Previous intraocular surgery or ocular trauma, hypersensitivity to NSAIDs.
All patients underwent complete ophthalmological examination,OCT, MF-ERG before phacoemulsification. Then, all patients were followed up 1d, 1wk, 1, 2, 3mo postoperative.
Group 1 received 0.1% nepafenac (nevanac, Alcon company).In pre-operative day, three times, in operative day, one hour before surgery every 15min. In postoperative, three times daily for one month. Group 2 did not receive nepafenac.
Phacoemulsification Phacoemulsification was done using stop and chop technique with intra-bagel posterior chamber foldable IOL implantation. All cataract surgeries were done by the same surgeon .
Before Phacoemulsification Pupil were dilated with(phenylephedrine 2.5% + tropicamide 1% + cyclopentolate 1%).Peribulbar anesthesia was done by using Mebevacaine HCL 3%. Sterilization of the skin was done with 10% povidene iodine and eyes were sterilized with povidene iodine 5%.
After Phacoemulsification Steroid-antibiotic drops 4 times daily for 2wk and then steroid was tapered over the next 3wk.
Optical Coherence Tomography OCT is a noninvasive and noncontact diagnostic tool with high resolution to assess macular changes[9]. Spectral-domain OCT scan of the macula was recorded using Topcon 3D 1000 OCT. After the patient scanning was finished, analysis protocol was used to obtain circular maps on the fovea. The macular retinal map divides the region into a central area with a radius of 500 microns, and two concentric rings inner perifoveal ring and outer parafoveal ring which were divided into four quadrants.
Multi-focal Electroretinogram MF-ERG is topographic map that records responses from central 30° the retina. This objective measurement was introduced because full-field electroretinography records mass responses from the whole retina[10]. Were recorded using Roland Consult, Brandenburg,Germany system were performed in accordance to ISCEV guidelines[11].
Dawson Trick litzkow (DTL) electrode was applied to topically anaesthetized cornea with one ground electrode on the forehead and two temporal reference electrodes. A stimulus array of 61 hexagons covering a visual field of 30o was presented on a monitor 30 cm from the eye. Each hexagon alternated between black and white. Subjects fixated at the center of the stimulus. The recording period was comprised of eight segments of 30s. Ring form and trace array were obtained. OCT and MF-ERG were done by the same person.Statistical Analysis Statistical analysis were analyzed by SPSS program versions 17 using Microsoft Windows 7.Parametric quantitative data were described using mean,standard deviation after testing normality using Kolmogrov-Smirnov test. Student’s t test and Mann-Whitney U test were used for comparison. Spearman correlation tests to correlate between variables. Significance of results was judged at the 5% level.
RESULTS
The study included 100 eyes of 100 diabetic patients with senile immature cataract. It included two groups. The demographic features presented in Table 1.
The best corrected visual acuity (BCVA) was statistically insignificant between two groups at preoperative and improved significantly at first week in two groups. There were no significant differences between two groups at the first two months. But, there was a statistically significant difference at three months postoperatively (P=0.05; Table 2).
Central macular thickness measured by OCT was statistically insignificant between two groups pre-operative. There was increase in macular thickness post-operative in Group 2 as compared to Group 1 (Table 3).
Five (5 eyes) of 50 eyes (10.0%) in Group 2 had macular edema >40 μm and no cases of edema observed in Group 1(Figures 1, 2).
There was increase in macular thickness (more than 30 µm and less than 40 µm) in 10 eyes (20%) in Group 1 and in 25 eyes(50%) in Group 2.
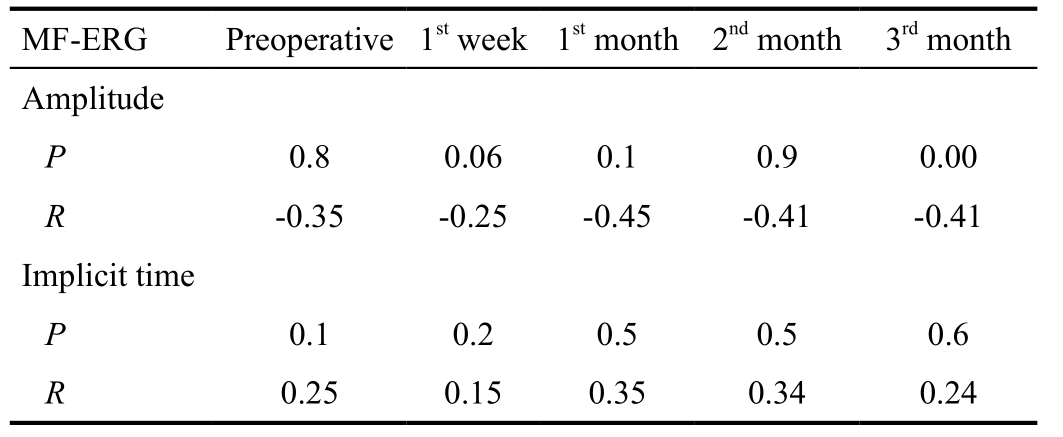
There were reduction of amplitude and delay in latencies in both groups. There were statistically insignificant differences between two groups. There was improvement of MF-ERG parameters postoperative. In early post-operative (first week and first month), there were increase in amplitude and reduction of latencies. There were insignificant differences between the two groups in the first two months. At third month,there were significant differences between two groups; there were reduction in amplitude and delay in latencies in Group 2 than in Group 1 (Table 4).

Figure 1 Normal OCT before phacoemulsification.
Table 1 Demographic features of groups n (%)
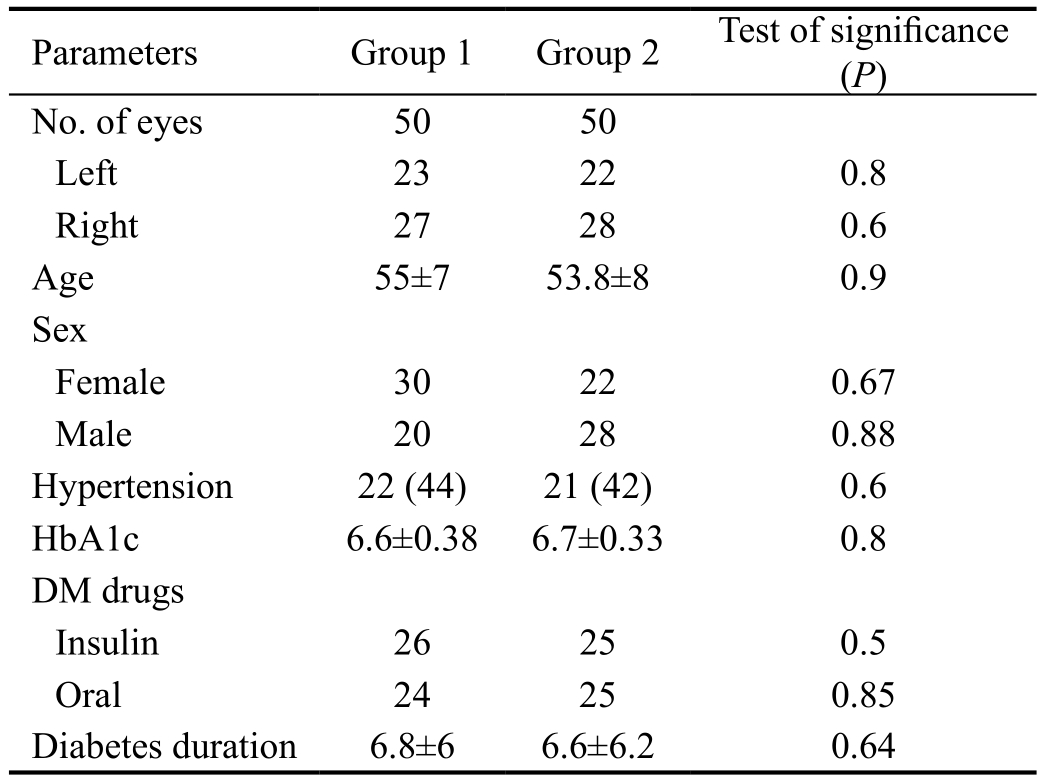
Parameters Group 1 Group 2 Test of significance(P)No. of eyes 50 50 Left 23 22 0.8 Right 27 28 0.6 Age 55±7 53.8±8 0.9 Sex Female 30 22 0.67 Male 20 28 0.88 Hypertension 22 (44) 21 (42) 0.6 HbA1c 6.6±0.38 6.7±0.33 0.8 DM drugs Insulin 26 25 0.5 Oral 24 25 0.85 Diabetes duration 6.8±6 6.6±6.2 0.64
Table 2 BCVA among groups
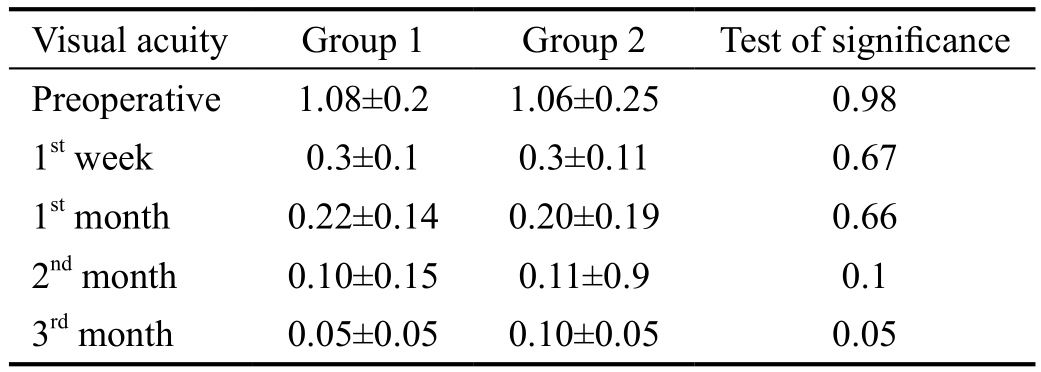
Visual acuity Group 1 Group 2 Test of significance Preoperative 1.08±0.2 1.06±0.25 0.98 1st week 0.3±0.1 0.3±0.11 0.67 1st month 0.22±0.14 0.20±0.19 0.66 2nd month 0.10±0.15 0.11±0.9 0.1 3rd month 0.05±0.05 0.10±0.05 0.05
Table 3 OCT changes among groups
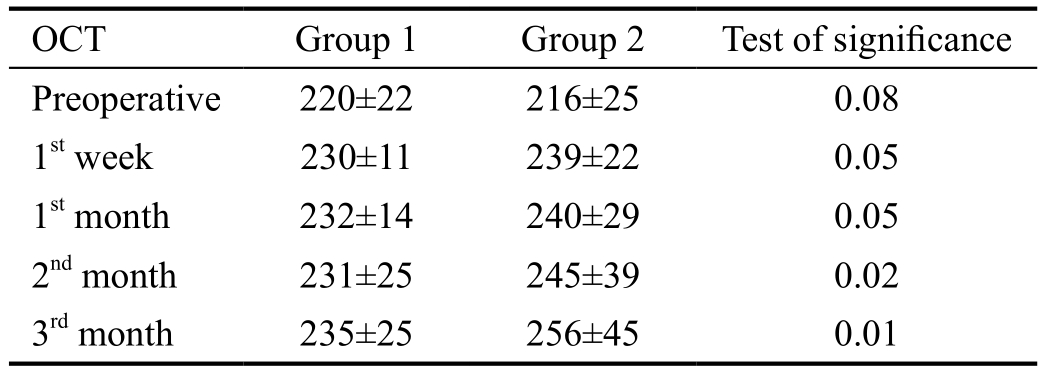
OCT Group 1 Group 2 Test of significance Preoperative 220±22 216±25 0.08 1st week 230±11 239±22 0.05 1st month 232±14 240±29 0.05 2nd month 231±25 245±39 0.02 3rd month 235±25 256±45 0.01
Table 4 MF-ERG changes in central rings among groups
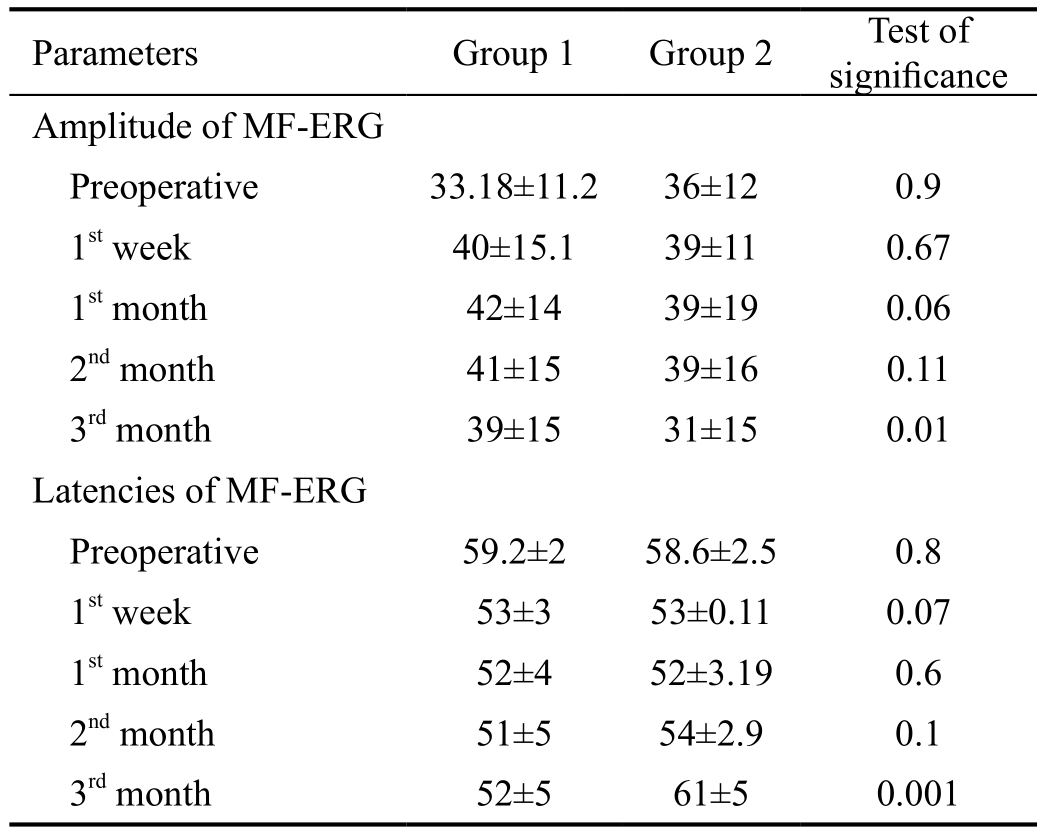
Parameters Group 1 Group 2 Test of significance Amplitude of MF-ERG Preoperative 33.18±11.2 36±12 0.9 1st week 40±15.1 39±11 0.67 1st month 42±14 39±19 0.06 2nd month 41±15 39±16 0.11 3rd month 39±15 31±15 0.01 Latencies of MF-ERG Preoperative 59.2±2 58.6±2.5 0.8 1st week 53±3 53±0.11 0.07 1st month 52±4 52±3.19 0.6 2nd month 51±5 54±2.9 0.1 3rd month 52±5 61±5 0.001
In cases developed CMO, There were marked reduction of amplitude and delay in latencies (Figures 3, 4).
There was significant correlation between macular thickness and BCVA in third month postoperative in Group 1 (R=0.5,P=0.005, R=0.6, P=0.004).
There was insignificant correlation between MF-ERG parameters and macular thickness (Table 5) except in five cases that developed CMO. There was significant correlation between MF-ERG amplitude and latencies and OCT macular thickness (R=0.55, P=0.005, R=0.52, P=0.004) respectively.There was moderate increase in macular thickness with reduction in amplitude and increase in latencies (Table 5).
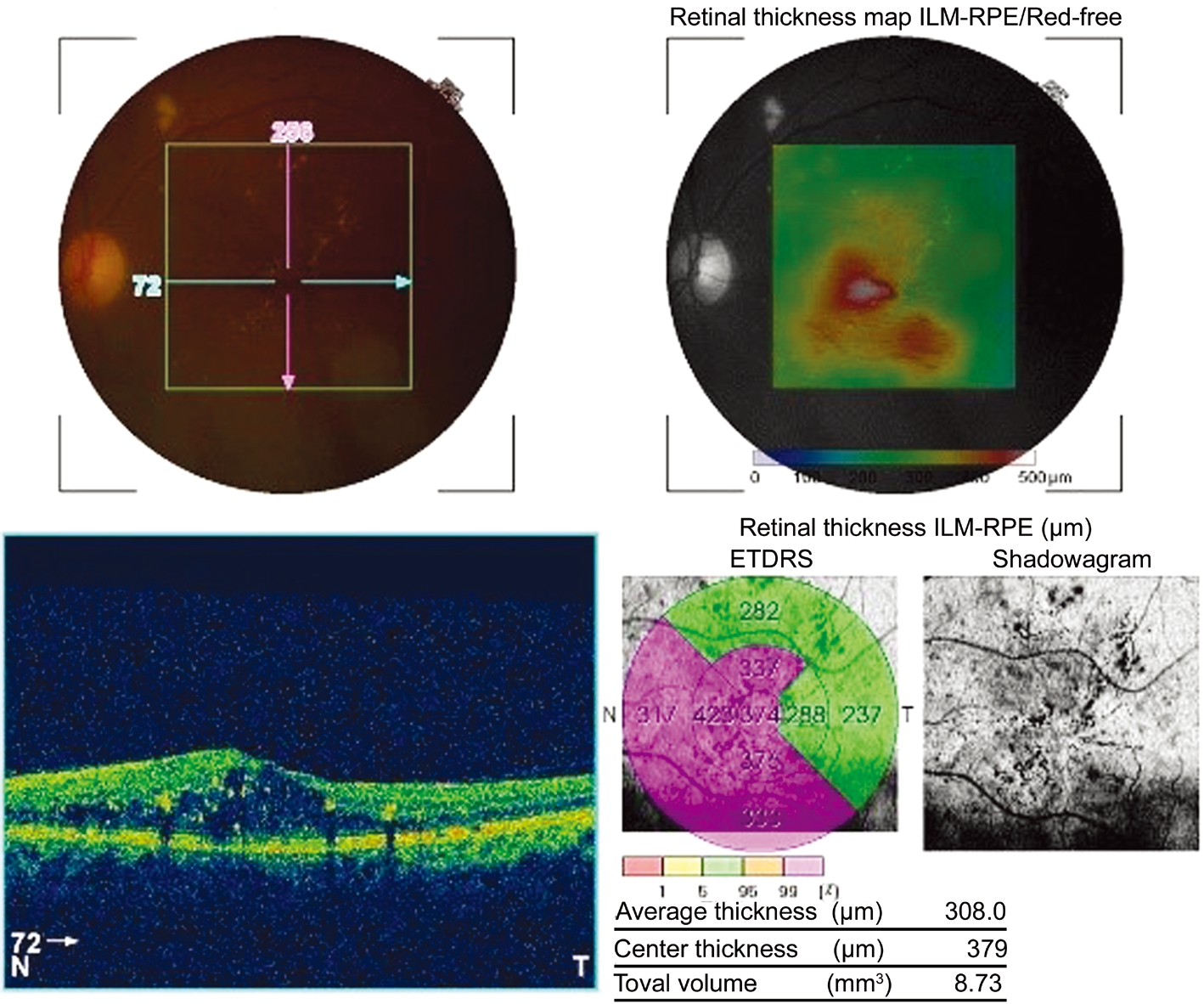
Figure 2 OCT shows CMO.
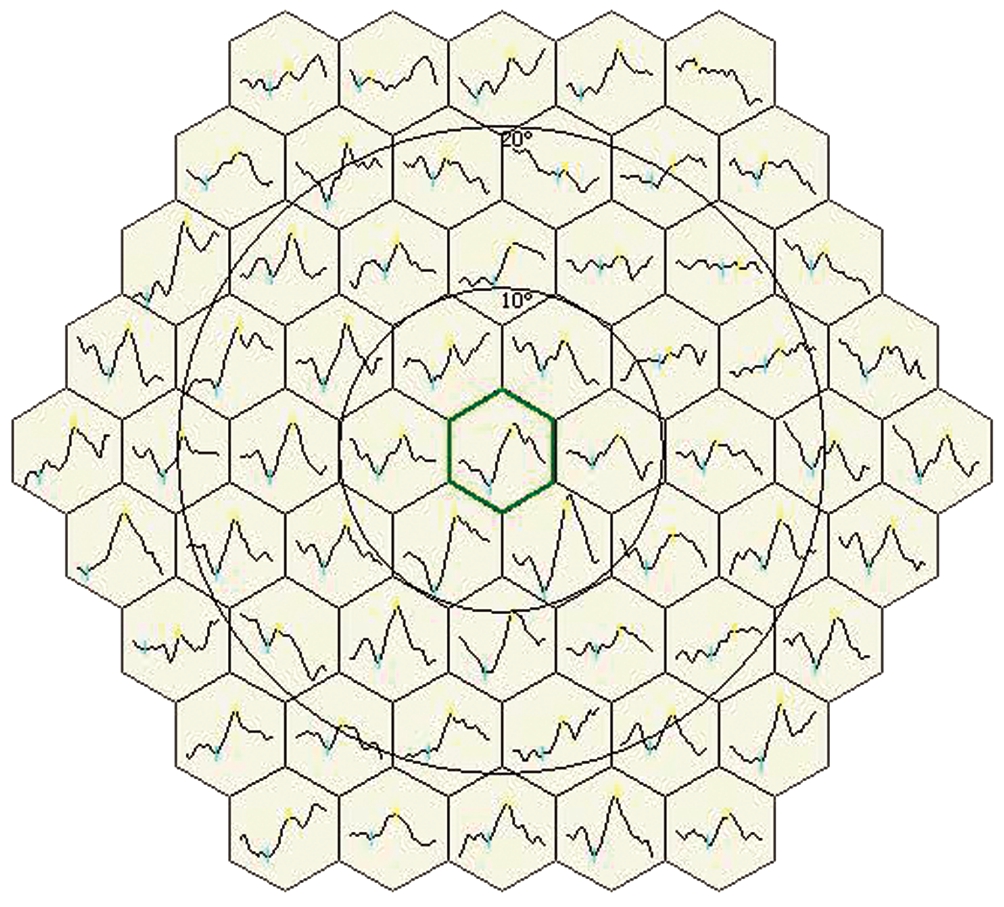
Figure 3 MF-ERG trace array before phacoemulsification (shows normal shape, normal amplitude and latency).
In Group 1 in our study, there is no case developed any complication related to nepafenac as: prolonged bleeding time,keratitis, epithelial breakdown, delayed wound healing or hypersensitivity.
DISCUSSION
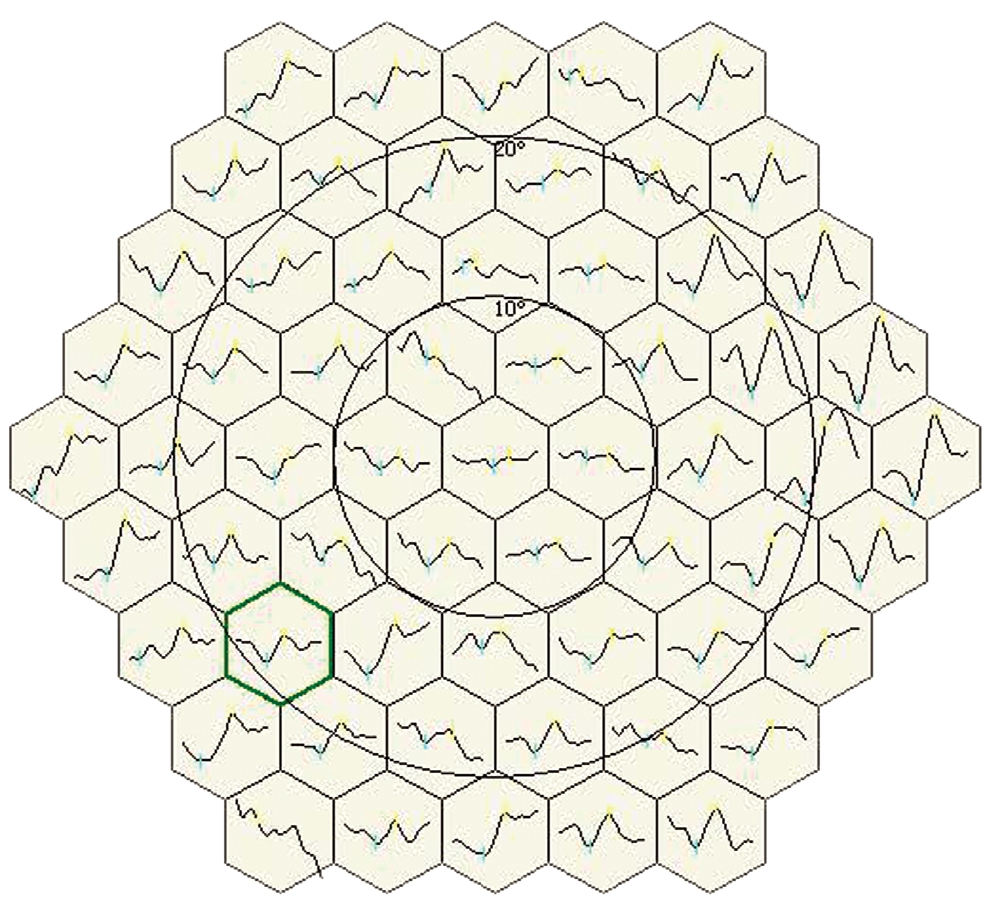
Figure 4 MF-ERG trace array after phacoemulsification (shows abnormal shape, decrease in amplitude and delay in latency).
Table 5 Correlation between CMT and MF-ERG in Group 1
?
Sub-clinical CMO is diagnosed as leakage from perifoveal dilated capillaries with fluorescein angiography without visual acuity affection after uncomplicated phacoemulsification in healthy individuals the incidence of sub-clinical CMO was less than 20%[1]. Clinical CMO can be identified on bio-microscopic examination and is associated with decreased visual acuity. After phacoemulsification surgery clinical CME has been reported to be less than 3% in healthy patients[12].
This study evaluated the value of addition of perioperative topical nepafenac to standard regimen of topical corticosteroids after uncomplicated phacoemulsification on central macular thickness, and retinal function in diabetic patient without diabetic changes. The study was performed on diabetic cataractous eyes because diabetes is risk factor for occurrence of CMO after cataract extraction in eyes with and without diabetic retinopathy[13]. In this study, there were five eyes(10%) developed clinical CMO (increase central macular thickness >40 µm from preoperative baseline) in Group 2(did not receive nepafenac) in contrast to Group 1 (received perioperative nepafenac). There was no eye develop CMO in Group 1.
Wittpenn et al[14] was reported occurrence of CMO in only 1.8% in control group after uncomplicated phacoemulsification surgery. This is much lower than reported in this study (10%).The cause of low incidence of CMO in Wittpenn et al’s study[14] was he evaluated the occurrence of CMO in low risk eyes for only one month while in this study we study the occurrence of CMO in high risk eyes (diabetic eyes) and for three months follow up. While, Singh et al[15] reported macular thickening more than 30 µm in 16.7% of patients in control group versus 2.4% in nepafenac group. He demonstrated the effect of nepafenac on 263 non-proliferative diabetic retinopathy patients began one day preoperatively and was continued for 90d follow up.
Also, Wolf et al[16] reported a significantly higher incidence of visually significant pseudophakic macular edema in patients treated with topical prednisolone alone after uneventful cataract surgery than those treated with topical prednisolone and nepafenac. Similarly, Kessel et al[17] found that the prevalence of postoperative CME was significantly higher in the steroid group than in the NSAIDs group: 25.3% versus 3.8% of patients. This study recommends using topical NSAIDs to prevent inflammation and macular edema after routine cataract surgery. That study was differ from our study as he exclude high risk patients.
Also, Tzelikis et al[18] concluded that nepafenac 0.3% was better in reducing macular thickness than placebo 5wk postoperatively without a difference in vision. Singh et al[19] reported that nepafenac 0.1% is effective in reducing postoperative CME and improvement of vision after cataract operation in diabetic patients. Yüksel et al[20] found that once-daily of nepafenac 0.3% may improve postoperative CMO in patients with high risk. Alnagdy et al[21] observed that preoperative and postoperative non-steroid anti-inflammatory reduce the frequency and severity of CME in diabetic eyes following phacoemulsification. Acar et al[22] reported that ketorolac and nepafenac decreased PGs level in both the aqueous and vitreous humors of rabbits. But, nepafenac was more effective than ketorolac in the vitreous.
In contrast, Tzelikis et al[23] reported that use of prophylactic ketorolac or nepafenac was not effective in prevention of macular thickening after uneventful cataract surgery compared with placebo. A database study of about 81 thousand eyes from patients with diabetes documented that increase risk of postoperative macular edema after surgery even in absence of diabetic retinopathy[24].
Also, multicenter database study across 19 centers from an electronic medical record system including 4850 eyes undergoing cataract surgery in patients with diabetes with no history of diabetic macular edema (DMO) demonstrated increase the rate of DMO that requiring treatment for one year postoperative. Risk of treatment-requiring DMO differed according to preoperative grade of retinopathy: being 1.0%in diabetic patients without diabetic retinopathy, 5.4% in mild non-proliferative diabetic retinopathy (NPDR), 10.0%in moderate NPDR, 13.1% in severe NPDR and 4.9% in proliferative diabetic retinopathy[25].
In contrast to this database, this study documented increase risk of treatment requiring CME to 10%. Our study was of limited number and diabetic patients were without diabetic retinopathy. Hayashi et al[13] found that, the degree of changes of DMO is more prominent in eyes with DR than in eyes without DR. Macular edema increases up to 3mo after cataract surgery, but thereafter decreases gradually.
In the present study all cases had no diabetic retinopathy preoperatively and macular thickening was reported postoperatively statistically significant in Group 2 than Group 1.There were reduction in amplitude with delay in latencies in both groups preoperatively due to lens opacity and diabetes.There were improvement of latencies and increase in amplitude postoperative in both groups due to removal of cataract. There were insignificant differences between both groups in the first two months. There was marked reduction of amplitude with increase in latency in Group 2 in cases of CMO.
Also, Bearse et al[26] found delay in latencies with and without reduction in amplitude in diabetes even in eyes without diabetic retinopathy. Gerth et al[27] reported reduction in MFERG values in opaque media due to reduction in illumination reached retina.
ACKNOWLEDGEMENTS
Conflicts of Interest: Mokbel T, None; Saleh S, None;Abdelkader M, None; El-khouly SE, None; Abou Samra W,None; Mamdouh M, None.
1 Mentes J, Erakgun T, Afrashi F, Kerci G. Incidence of cystoid macular edema after uncomplicated phacoemulsification. Ophthalmologica 2003;217(6):408-412.
2 Mathys KC, Cohen KL. Impact of nepafenac 0.1% on macular thickness and postoperative visual acuity after cataract surgery in patients at low risk for cystoid macular oedema. Eye (Lond) 2010;24(1):90-96.
3 Elsawy MF, Badawi N, Khairy HA. Prophylactic postoperative ketorolac improves outcomes in diabetic patients assigned for cataract surgery. Clin Ophthalmol 2013;7:1245-1249.
4 Loewenstein A, Zur D. Postsurgical Cystoid Macular Edema//Loewenstein A, Zur D. eds. Macular Edema. Basel: KARGER, 2010:148-159.
5 Flesner P, Sander B, Henning V, Parving HH, Dornonville de la Cour M, Lund-Andersen H. Cataract surgery on diabetic patients. A prospective evaluation of risk factors and complications. Acta Ophthalmol Scand 2002;80(1):19-24.
6 Kim SJ, Flach AJ, Jampol LM. Nonsteroidal anti-inflammatory drugs in ophthalmology. Surv Ophthalmol 2010;55(2):108-133.
7 Bucci FA Jr, Waterbury LD, Amico LM. Prostaglandin E2 inhibition and aqueous concentration of ketorolac 0.4% (acular LS) and nepafenac 0.1%(nevanac) in patients undergoing phacoemulsification. Am J Ophthalmol 2007;144(1):146-147.
8 Ahuja M, Dhake AS, Sharma SK, Majumdar DK. Topical ocular delivery of NSAIDs. AAPS J 2008;10(2):229-241.
9 Tátrai E, Ranganathan S, Ferencz M, DeBuc DC, Somfai GM.Comparison of retinal thickness by Fourier-domain optical coherence tomography and OCT retinal image analysis software segmentation analysis derived from Stratus optical coherence tomography images. J Biomed Opt 2011;16(5):056004.
10 Lung JC, Swann PG, Chan HH. Early local functional changes in the human diabetic retina: a global flash multifocal electroretinogram study.Graefes Arch Clin Exp Ophthalmol 2012;250(12):1745-1754.
11 McCulloch DL, Marmor MF, Brigell MG, Hamilton R, Holder GE,Tzekov R, Bach M. Erratum to: ISCEV Standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol 2015;131(1):81-83.
12 Lobo C. Pseudophakic cystoid macular edema. Ophthalmologica 2012;227(2):61-67.
13 Hayashi K, Igarashi C, Hirata A, Hayashi H. Changes in diabetic macular oedema after phacoemulsification surgery. Eye (Lond)2009;23(2):389-396.
14 Wittpenn JR, Silverstein S, Heier J, Kenyon KR, Hunkeler JD, Earl M, Acular LS for Cystoid Macular Edema (ACME) Study Group. A randomized, masked comparison of topical ketorolac 0.4% plus steroid vs steroid alone in low-risk cataract surgery patients. Am J Ophthalmol 2008;146(4):554-560.
15 Singh R, Alpern L, Jaffe GJ, Lehmann RP, Lim J, Reiser HJ, Sall K,Walters T, Sager D. Evaluation of nepafenac in prevention of macular edema following cataract surgery in patients with diabetic retinopathy.Clin Ophthalmol 2012;6:1259-1269.
16 Wolf EJ, Braunstein A, Shih C, Braunstein RE. Incidence of visually significant pseudophakic macular edema after uneventful phacoemulsification in patients treated with nepafenac. J Cataract Refract Surg 2007;33(9):1546-1549.
17 Kessel L, Tendal B, Jørgensen KJ, Erngaard D, Flesner P, Andresen JL,Hjortdal J. Post-cataract prevention of inflammation and macular edema by steroid and nonsteroidal anti-inflammatory eye drops: a systematic review. Ophthalmology 2014;121(10):1915-1924.
18 Tzelikis PF, Morato CS, Neves NT, Hida WT, Alves MR. Intraindividual comparison of nepafenac 0.3% for the prevention of macular edema after phacoemulsification. J Cataract Refract Surg 2018;44(4):440-446.
19 Singh RP, Staurenghi G, Pollack A, Adewale A, Walker TM, Sager D, Lehmann R. Efficacy of nepafenac ophthalmic suspension 0.1%in improving clinical outcomes following cataract surgery in patients with diabetes: an analysis of two randomized studies. Clin Ophthalmol 2017;11:1021-1029.
20 Yüksel B, Karti Ö, Kusbeci T. Topical nepafenac for prevention of post-cataract surgery macular edema in diabetic patients: patient selection and perspectives. Clin Ophthalmol 2017;11:2183-2190.
21 Alnagdy AA, Abouelkheir HY, El-Khouly SE, Tarshouby SM. Impact of topical nonsteroidal anti-inflammatory drugs in prevention of macular edema following cataract surgery in diabetic patients. Int J Ophthalmol 2018;11(4):616-622.
22 Acar U, Acar DE, Tanriverdi C, Acar M, Ozdemir O, Erikci A, Ornek F. Prostaglandin E2 levels of aqueous and vitreous humor in ketorolac 0.4% and nepafenac 0.1% administered healthy rabbits. Ocul Immunol Inflamm 2017;25(3):323-327.
23 Tzelikis PF, Vieira M, Hida WT, Motta AF, Nakano CT, Nakano EM, Alves MR. Comparison of ketorolac 0.4% and nepafenac 0.1% for the prevention of cystoid macular oedema after phacoemulsification:prospective placebo-controlled randomised study. Br J Ophthalmol 2015;99(5):654-658.
24 Chu CJ, Johnston RL, Buscombe C, Sallam AB, Mohamed Q, Yang YC, United Kingdom Pseudophakic Macular Edema Study Group. Risk factors and incidence of macular edema after cataract surgery: a database study of 81984 eyes. Ophthalmology 2016;123(2):316-323.
25 Denniston AK, Chakravarthy U, Zhu HG, et al. The UK Diabetic Retinopathy Electronic Medical Record (UK DR EMR) Users Group,Report 2: real-world data for the impact of cataract surgery on diabetic macular oedema. Br J Ophthalmol 2017;101(12):1673-1678.
26 Bearse MA, Han Y, Schneck ME, Barez S, Jacobsen C, Adams AJ. Comparison of fast and slow flash multifocal electroretinogram techniques: prediction of non proliferative diabetic retinopathy development.Invest Ophthalmol Vis Sci 2005;46:(13):1.
27 Gerth C, Garcia SM, Ma L, Keltner JL, Werner JS. Multifocal electroretinogram: age-related changes for different luminance levels.Graefes Arch Clin Exp Ophthalmol 2002;240(3):202-208.