·Clinical
Research·
Unilateral
foveomacular retinitis resembling solar retinopathy among young soldiers in
Korean army and associated multimodal imaging findings
Chang
Ki Yoon1,2, Kyu Hyung Park1, Se Joon Woo1
1Department of Ophthalmology, Seoul National
University College of Medicine, Seoul National University Bundang Hospital,
Seongnam 13620, Korea
2Department of Ophthalmology, Hallym
University College of Medicine, Hallym University Kangnam Sacred Heart
Hospital, Seoul 07441, Korea
Correspondence to: Se Joon Woo. Department of
Ophthalmology, Seoul National University Bundang Hospital, #82, Gumi-ro
173beon-gil, Bundang-gu, Seongnam-si, Gyeonggi-do 13620, Korea.
sejoon1@snu.ac.kr
Received: 2019-09-20
Accepted: 2019-11-05
Abstract
AIM: To describe the
clinical features and multimodal images of unilateral foveomacular retinitis in
young Korean soldiers.
METHODS: Ten patients having
foveomacular retinitis were included. Fluorescein angiography, fundus
autofluorescence (FAF), infrared reflectance (IR), and spectral-domain optical
coherence tomography (SD-OCT) were analyzed.
RESULTS: All patients were
young males experienced insidious visual decline without exposure to bright
light. Initial and final vision ranged from hand movement to 20/20 (median
20/200) and 20/2000 to 20/20 (median 20/500), respectively. Vision decreased in
6 patients while improved in two. Typical macular abnormality was yellow
granular spots. SD-OCT showed ellipsoid zone (EZ) or interdigitation zone (IZ)
disruption of fovea. The degree of EZ/IZ damage correlated with vision. Lesions
were clearly visualized through IR and matched with SD-OCT findings.
CONCLUSION: This is the first case
series of foveomacular retinitis diagnosed with multimodal imaging.
Foveomacular retinitis should be suspected in sudden unilateral visual decline
especially in young soldiers. SD-OCT is the most important diagnostic modality.
KEYWORDS: foveomacular
retinitis; Korean; multimodal; imaging; solar retinopathy; soldiers; unilateral
DOI:10.18240/ijo.2020.01.16
Citation: Yoon
CK, Park KH, Woo SJ. Unilateral foveomacular retinitis resembling solar
retinopathy among young soldiers in Korean army and associated multimodal
imaging findings. Int J Ophthalmol 2020;13(1):112-119
INTRODUCTION
Foveomacular retinitis is a term
used to describe an eye disease characterized by central vision loss from a
foveal retinitis which subsequently develops into a foveal cyst or hole. It was
first reported in naval personnel and has been mostly reported and studied in
the military field[1]. As the fundus appearance of
foveomacular retinitis is similar to that of solar retinopathy, it was often
regarded as synonymous to solar retinopathy. However, it mostly appears in
patients who deny history of exposure to bright light. Besides it has been
reported that foveomacular retinitis shows different clinical course and
distinct morphologic features from solar retinopathy. Therefore, the
pathogenesis of foveomacular retinitis remains poorly understood, not like
solar retinopathy.
We recently evaluated 10 patients
having foveomacular retinitis from among young Korean soldiers who were
referred from the military hospital of South Korea. The patients complained of
unilateral visual decline with distinct macular abnormality. Herein, we present
the detailed clinical course, including multimodal imaging features, of 10
patients with foveomacular retinitis.
SUBJECTS AND METHODS
Ethical Approval All study conduct adhered to the
tenets of the Declaration of Helsinki (Edinburgh, 2000) and the study protocol
was approved by the Institutional Review Board of the Seoul National University
Bundang Hospital. This was a retrospective study and informed consent was not
from patients.
All patients were enlisted personnel
who visited the Armed Forces Capital Hospital (AFCH) of South Korea between
November 2010 and June 2014, and were referred to the Retina Clinic in Seoul
National University Bundang Hospital (SNUBH). All patients underwent a thorough
ophthalmologic examination including fundus color photography, fluorescein
angiography (FA), and spectral-domain optical coherence tomography (SD-OCT).
Visual field test, electroretinography, and multifocal electroretinography were
performed in selected cases. The Cirrus SD-OCT (Carl Zeiss Meditech Inc.,
Dublin, California, USA) was used to obtain the SD-OCT images. Additionally,
Spectralis OCT (Heidelberg Engineering, Heidelberg, Germany) and infrared
reflectance (IR; 820 nm) imaging were performed on 7 patients (Cases 1, 3, 4,
5, 7, 9, and 10). Blue-light fundus autofluorescence (FAF; 488 nm) images were
obtained for 4 patients (Cases 1, 4, 7, and 10) using Heidelberg retinal
angiography (HRA, Heidelberg Engineering, Heidelberg, Germany). Central foveal
thickness was measured using the caliper tool provided in the Cirrus SD-OCT
software. The best corrected visual acuity (BCVA) was measured with a standard
Korean Landolt visual acuity chart, and the decimal visual acuity was converted
to the logarithm of the minimal angle resolution (logMAR) units for statistical
analyses.
RESULTS
All ten patients were male and
ranged from 19 to 22y in age (mean 20.0±1.0y). All patients presented with
unilateral central visual disturbances such as central scotoma, blurred vision,
or metamorphopsia. Every patient denied the history of bright light exposure
such as sun-gazing, laser injury, sunbathing or arc welding and significant
trauma. None of the patients could recollect any coexisting viral infection or
family history of retinal disease and were taking any medication concurrently.
Only one patient (Case 3) was participating in regular military training at the
time of onset. Others recollected no hard, outdoor physical drill around the
time of onset of symptoms. All patients had been assigned to ground duties. The
clinical features of a representative case (Case 7) are presented in Figure 1
and the clinical characteristics of all patients and involved eyes are
summarized in Table 1.
Visual acuity at presentation varied
between hand movement and 20/20 (median 20/200, average 20/160). The average
visual acuity at final follow-up was 20/350 (average follow-up period: 10.1mo).
Visual acuity decreased in 6 patients and improved in 2 patients finally (from
20/32 to 20/25 in one
case and hand movement to 20/1000 in
another). The mean±standard deviation (SD) central foveal thickness was
191.3±8.7 µm in the diseased eyes and 211.6±10.0 µm in the contralateral
healthy eyes (P=0.005, Wilcoxon signed rank test). On fundus
photography, retinal lesions were usually located in the central macula area:
one or more small yellow granular spots with unclear margins were visible in
the foveal region. Large confluent granular yellow lesioin with surrounding
geographic depigmentation were seen only in Case 10. FA up of mid
arteriovenouse phase showed hyperfluorescence from retinal pigment epithelium
(RPE) atrophy in Cases 2, 5, and 7 (Figures 1 and 2). Unlike these, confluent
hypofluorescence with surrounding hyperfluorescence was observed in case 10
(Figure 3). In other 6 patients, abnormal findings were not detected on FA.
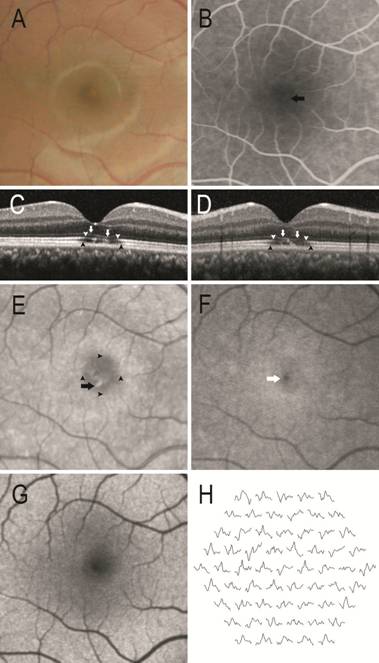
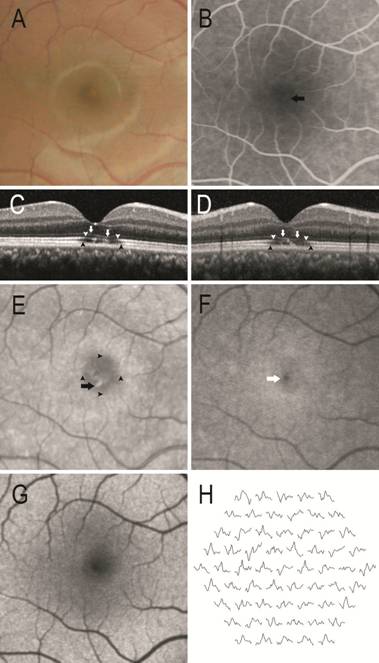
Figure 1 Results of ophthalmologic
examination of a representative case (Case 7) who presented with a visual
acuity of 20/200 A: Color fundus photography showing a small foveal
yellow granular spot with surrounding pigment mottling. B: FA showing a mild
transmission defect (arrow). C, D: SD-OCT showing external limiting membrane
depression (white arrow), EZ defect and fragmentation (white arrowhead), and IZ
defect (black arrowhead). Horizontal scan (C) and vertical scan (D). E: IR
image (820 nm) showing a granular pattern of hyperreflectivity at the central
fovea (arrow) and an enlarged foveal hyporeflective signal (arrowhead). This
alteration is more prominent than in the fundus photograph. F: Blue peak
reflectance showing hyper-reflective lesion at fovea (white arrow). G:
Blue-light autofluorescence image is unremarkable. H: Multifocal
electroretinography displaying decreased amplitudes at central retinal areas.
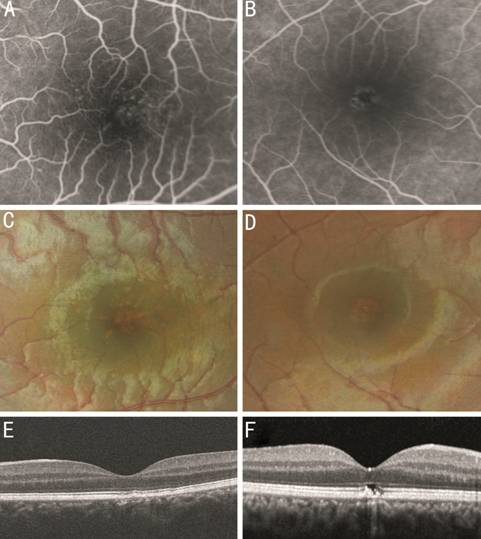
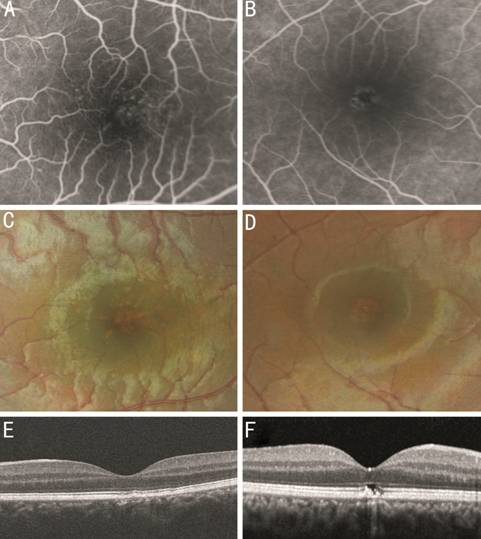
Figure 2 Fluorescein angiogram,
fundus photograph, and SD-OCT A, C and E: Case 2. A speckled
pattern of transmission defects on FA and corresponding pigment mottling on
fundus photography are observed. The lesion corresponds to the decreased EZ and
RPE reflectivity on OCT. B, D, and F: Case 5. A ring-shaped transmission defect
and corresponding pigment mottling are observed. The lesion also coincides with
EZ and RPE defect on OCT.
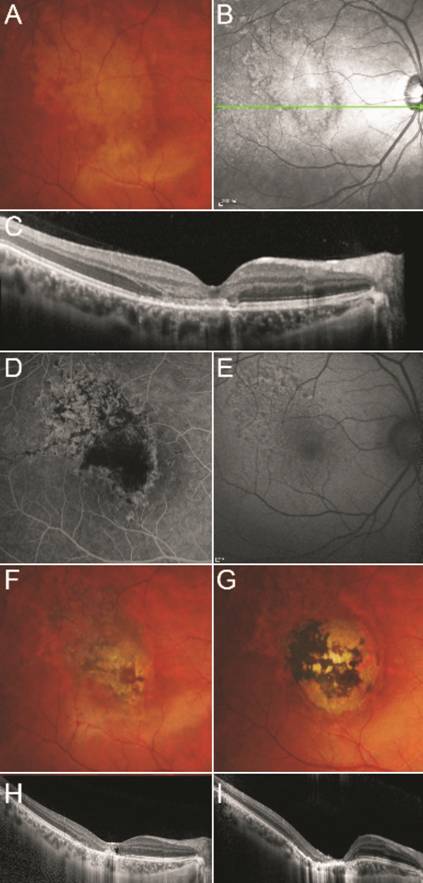
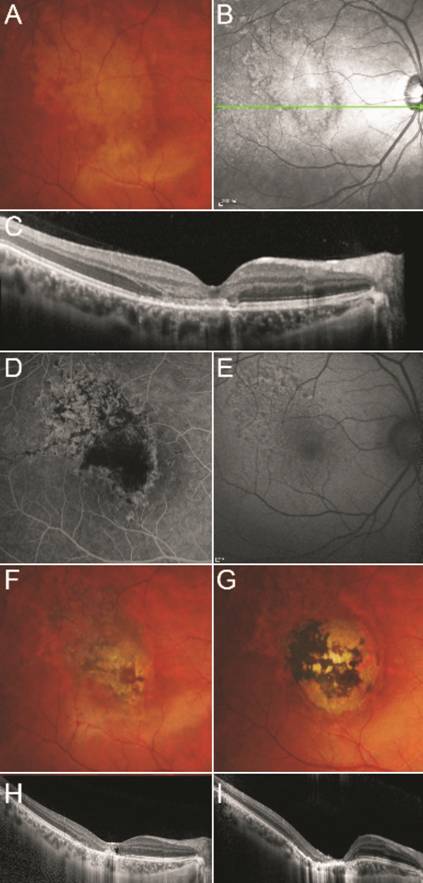
Figure 3 Case 10 A: Fundus photography at first visit shows yellow
hypopigmented geographic lesion at macula. IR images (B) and OCT (C) at first
visit. Hyperreflective lesion is well visualized and the margin of the lesion
is delineated sharply with hyporefective line in FAF. On OCT, thinning in the
outer nuclear layer and disruption of photoreceptor layers are observed. A
hyperreflective band continuous with external limiting membrane is detected.
Fundus FA (D) 1mo after first visit, showing tissue defect. FAF image (E) and
fundus photography (F) at 2mo shows central dark pigmentation and RPE atrophy.
H: OCT at 2mo shows outer retinal disruption, hyperreflective dots, and cysts
in the fovea. G: Fundus photography after 1y shows central dark pigmentation
and surrounding circular chorioretinal atrophy. I: OCT shows progression of
outer retinal layer thinning. FCE and choroidal thinning have developed and the
choroidal lesion corresponds to the round atrophic lesion seen in fundus
photography.
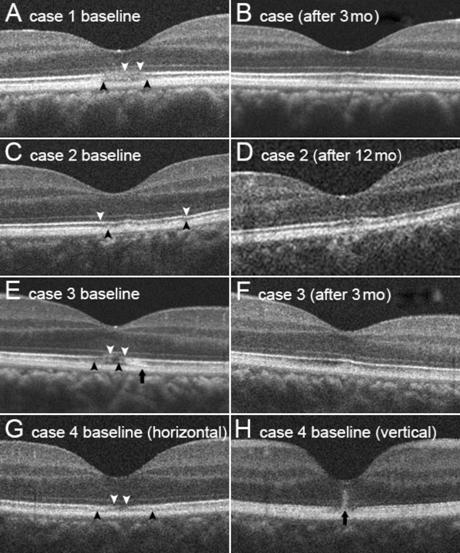
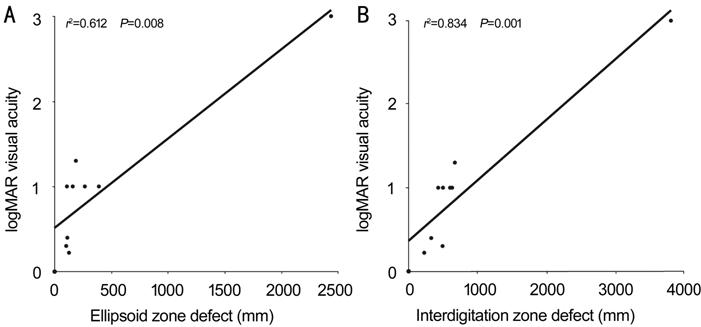
The SD-OCT images showed varying
degrees of photoreceptor disruption in all cases. The cases were categorized
into two groups based on the severity of photoreceptor disruption. The mild
group showed photoreceptor layer blurring with a relatively preserved ellipsoid
zone (EZ) (Group 1; Cases 1, 2, 3, and 4; Figure 4) and the severe group had
discrete photoreceptor layer defect involving EZ (Group 2; Cases 5, 6, 7, 8, 9,
and 10; Figure 5). Case 5 showed a unique, hyperreflective, central columnar
structure, which disappeared after 8mo. In Group 1, the EZ was relatively
preserved and visual acuity was better than in Group 2 (20/30 vs 20/500
respectively, P=0.011 Wilcoxon rank sum test). The logMAR visual acuity
correlated with the photoreceptor defect size in the EZ and interdigitation
zone (IZ) (EZ vs logMAR, R2=0.612, P=0.008; IZ vs
logMAR, R2=0.834, P<0.001, Spearman correlation;
Figure 6). The visual acuity improved in Cases 3 and 10, was maintained in Case
2 of Group 1 and declined in all other cases. However, during follow-up, outer
retinal contour disruption recovered and EZ defect size decreased in Cases 1,
3, 5, 6, and 7. In Case 10, thickened outer plexiform layer and a
hyperreflective band continuous with the external limiting membrane were
observed; focal choroidal excavation (FCE) gradually developed during 3y of
follow-up (Figure 3).
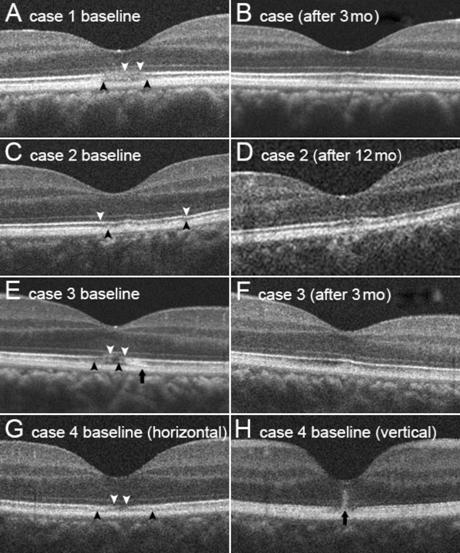
Figure 4 SD-OCT images of cases that
presented with photoreceptor layer blurring with relatively preserved EZ (Group
1) Despite EZ blurring, EZ band is dimly
visible in all cases. B, D, and F are follow-up images of A, C, and E images.
Follow-up images of B, D, and F were taken at 3, 12, and 3mo, respectively.
White arrowheads: EZ defect area; Black arrowheads: IZ defect. EZ and IZ
blurring and defects show improvement in the follow-up images. The black
arrows (E) indicate abnormal
hyperreflectivity at the photoreceptor layer. This hyperreflectivity decreased
during the follow-up. G and H are the initial OCT images (horizontal and
vertical scans) of Case 4 because consecutive photo was not obtained. Central
hyperreflective columnar structure is observed with surrounding hyporeflective
area (black arrow).
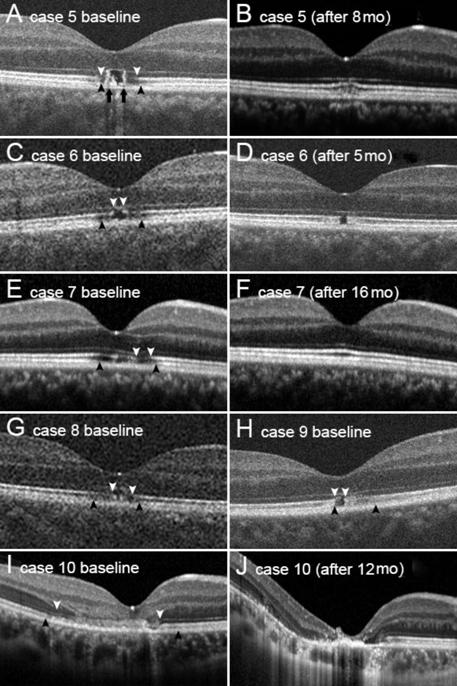
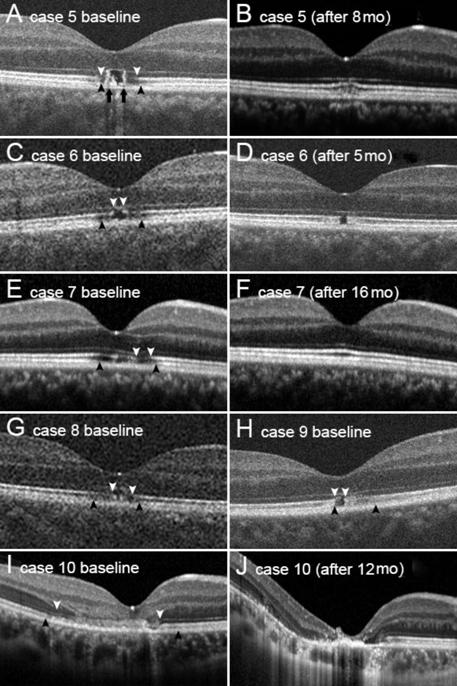
Figure 5 SD-OCT images of cases that
presented with discrete photoreceptor layer defects involving EZ (Group 2) A, C, E, G, H, I: The baseline images
show severe outer retinal defects and surrounding hyporeflective areas with
discontinuation of EZ. B, D, F, J: The follow-up images of Cases 5, 6, 7, and
10 taken after 8, 5, 16, and 12mo, respectively. White arrowheads: EZ defects;
Black arrowheads: IZ defects. The photoreceptor disruption recovered either
partly or completely, except in Case 10. Black arrows in image A indicate
hyperreflective columnar structure in the photoreceptor layer. I: Outer
plexiform layer is thickened but its margin is indistinct. Hyperreflective band
continuous with external limiting membrane is visible between white arrowheads.
J: Outer nuclear layer and outer plexifom layer are invisible; instead
hyperreflective material is detected at foveola. Choroidal curvature has become
steeper after a year.
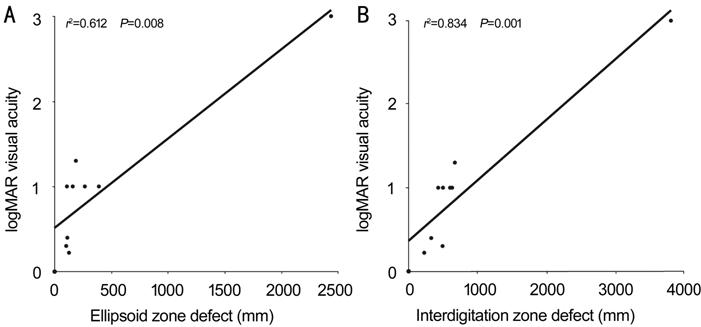
Figure 6 Correlation between size of
EZ defect and logMAR visual acuity (A) and between IZ defect size and logMAR
visual acuity (B) Visual acuity significantly
correlated with size of EZ and IZ defect. Outliers located at the right upper
corner in A and B, indicate Case 10.
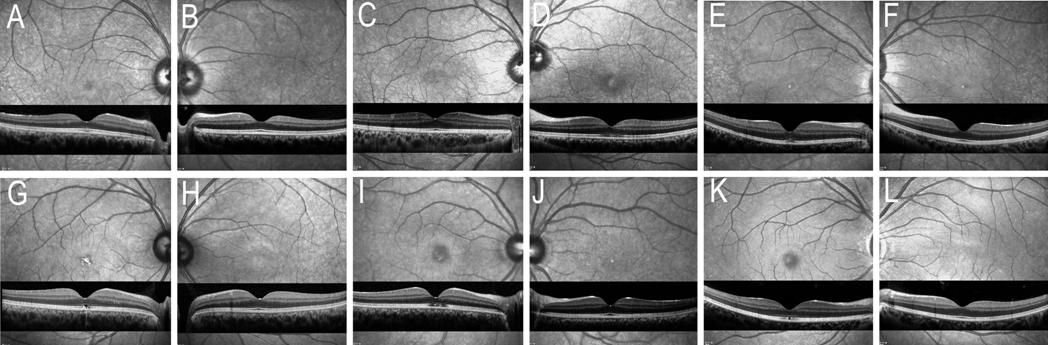
IR image revealed irregularly
increased reflectance signal at the fovea with surrounding low reflective ring
in six out of seven (85%) patients (Figures 3 and 7). In all cases, IR images
could better delineate the lesion than conventional fundus photography.
However, no abnormal finding on fundus IR was observed in the healthy
contralateral fellow eyes. FAF images revealed no remarkable findings in all
patients, except Case 10 (Figure 1) in which irregular hypofluorescent spots
were observed (Figure 3).
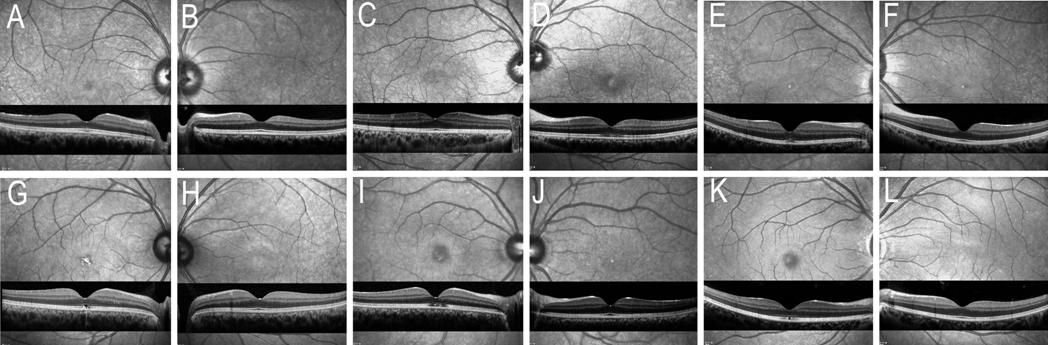
Figure 7 IR images (820 nm) of Case
1 (A and B), Case 3 (C and D), Case 4 (E and F), Case 5 (G and H), Case 7 (I
and J), and Case 9 (K and L) Increased reflectivity with
surrounding hyporeflective ring is observed in all cases except Case 4.
Corresponding OCT images are shown under the respective IR images. A, D, E, G,
I, and K are images of the involved eyes.
DISCUSSION
This is the first case series of
foveomacular retinitis in young male soldiers, that presents multimodal imaging
data, including high resolution SD-OCT. Typical yellow granular spots in the
fovea were observed on fundus photography. Photoreceptor disruption involving
IZ and/or EZ was observed on SD-OCT and visual loss correlated with OCT
features. Fundus IR imaging was also useful to detect the foveal lesions, while
FAF was not. Although photoreceptor disruption on SD-OCT improved either
partially or completely, visual acuity did not recover in most cases.
A red, sharply demarcated, foveal or
juxtafoveal spot located at the level of the outer retina is suggestive of
solar retinopathy[2]. In our cases, yellow spots
and pigment mottling were consistently observed. This ophthalmoscopic
appearance and the OCT findings resemble chronic solar retinopathy despite the
absence of direct sun gazing or sunbathing history. Several studies have
reported presumed solar retinopathy in patients who denied direct sun gazing.
Rai et al[3] reported that only 51% of
patients could recollect a history of sun-gazing. Following their suggestion,
absence of a history of sun viewing may not be sufficient to exclude solar
retinopathy. Generally, soldiers are more likely to be exposed to the sun than
civilians of the same age in industrialized nations. However, our patients were
not assigned to hard training unit performing a lot of outdoor work. All the
patients included in this series repeatedly denied sun gazing or bright light
exposure. Further, additional case was not reported in the same military units.
Our patients also denied using laser beam or welding arc which can produce
lesions similar to solar retinopathy[4]. Thus,
light-associated toxicity was probably not the relevant etiological factor in
our study.
Up to now, there have been two case
reports of OCT findings in foveomacular retinitis. Topouzis et al[5] described the localized loss of the RPE and
photoreceptor layers at fovea. Badhani et al[6]
reported 10-year-old boy with a full-thickness, rectangular, hyperreflective
lesion which was replaced by a sharp defect in the outer retina over the course
of five years. Regarding solar retinopathy, several studies have described OCT
findings. Entire retinal hyperreflectivity can appear for several days, which
corresponds to yellow retinal lesions in acute stage of solar retinopathy[7-9]. Other reports of chronic cases
revealed hyporeflective spaces in the outer retina which were more prominent on
SD-OCT[8,10-14].
Our patients showed hyporeflective areas limited to the outer retina, especially
the photoreceptor layer, while sparing the RPE layer. These OCT findings are
similar to those observed in chronic solar retinopathy. These are also
consistent with the OCT features in the two cases of foveomacular retinitis[5-6]. The hyporeflective photoreceptor
defect and EZ contour disruption recovered in all cases except Cases 2 and 10
(Cases 4, 8, and 9 had no follow-up OCT). We divided the hyporeflective pattern
into two groups and this classification correlated well with the degree of visual
impairment.
Interestingly, a hyperreflective
columnar structure was observed on OCT in Case 5 (Figure 5). Which is a similar
finding in acute solar retinopathy. This hyperreflective lesion is also
detected in a recently reported case of foveomacular retinitis[6]. Longitudinal observation revealed that the
hyperreflective band was detected at 1mo and resolved after 3mo. It seems that
this lesion may be an early OCT finding in both solar retinopathy and
foveomacular retinitis.
We observed FCE in Case 10. This
case had a severe form of foveomacular retinitis with poor visual outcome. FCE
has been reported in several retinal diseases including central serous
chorioretinopathy, multiple evanescent white dot syndrome, multifocal
choroiditis, punctate inner choroidopathy etc[15-17]. Although the exact mechanism of FCE has not been
clearly elucidated, our case indicates that localized choroidal damage and
atrophic thinning may play a role. To the best of our knowledge, this is the
first case showing FCE development in case of foveomacular retinitis.
IR images in our cases revealed more
visible alteration than conventional color fundus images and the abnormality
was observed only in the affected eyes. Issa et al[18]
have reported similar IR findings in solar retinopathy. They also reported
increased foveal reflectance/fluorescence with blue reflectance (488 nm) and
blue-light autofluorescence (488 nm) and the foveal abnormality was also found
in the healthy fellow eyes. However, in the present study, the fellow eyes showed
no abnormality on any imaging examinations. Ahn et al[19]
also showed a macular abnormality on IR images in occult macular dystrophy that
could not be detected on fundus photography. Taken together, IR imaging is
useful for detecting subtle foveal abnormalities in foveomacular retinitis that
might be difficult to detect on color fundus photography.
Solar retinopathy usually occurs
bilaterally[20]. Sometimes, patients with
eccentric fixation or uniocular occlusion can show unilateral involvement.
Foveomacular retinitis has been known to involve both eyes at variable rates
from 30% to 100%[1,20]. Marlor et
al[21] reported sequential involvement of
both eyes in some patients. In contrast, our cases presented exclusively with
unilateral lesions and there was no sequential involvement of the other eye.
None of the patients in our series evinced eccentric fixation or large angle
strabismus. Therefore, absence of bright light exposure history andunilateral
involvement in orthotropic patients supports a diagnosis of foveomacular
retinitis rather than light exposure associated retinopathy.
Retinal diseases reported in young
soldiers are mostly associated with trauma, hard exercise, flight, etc[22-24]. In our cases however,
traumatic maculopathy, whiplash maculopathy, and toxic maculopathy can be
excluded as all patients denied relevent histories. Another possible
differential diagnosis is unilateral acute idiopathic maculopathy (UAIM), a
rare disorder presenting with transient visual loss in a young patient secondary
to exudative macular detachment and infiltrates, preceded by a viral infection[25]. Although unilateral involvement in young healthy
adults matches the clinical profile of our patients, viral prodrome and
complete recovery of vision in UAIM differ. Recent reports on UAIM have
described similar photoreceptor EZ loss on SD-OCT[26-27]. However, RPE hyperreflectivity on SD-OCT and macula
hypofluorescence on FA also reported in UAIM were not observed in any of our
cases. Acute retinal pigment epitheliitis (ARPE) affects healthy young adults
with the symptom of painless blurring or vision loss and should also be ruled
out[28-29]. The SD-OCT
findings in ARPE include inner RPE involvement, disruption of IS, a dome-shape
hyperreflective lesion at the outer retina, and external limiting membrane
displacement. The condition is usually unilateral and shows visual improvement
within 3mo. However, in our cases, the RPE layer was spared and no substantial
visual recovery occurred despite noticeable resolution of photoreceptor lesions
on OCT.
Foveomacular retinitis has been
reported to show variable degrees of visual decline[1,21]. Marlor et al[21]
reported that 32% (89 out of 274) had 20/200 or worse vision and only 5% (14 out
of 274) had 20/40 or better vision at the time of discharge. Among patients with
poor vision at presentation (≤20/200), 46% (15 out of 70) showed visual improvement
while 67% (6 out of 9) of those with good visual acuity (≥20/40) showed visual
decline during 5y of follow-up. In our cases, 8 of 10 patients (80%) had
reached lower than 20/200 vision and only two patients showed visual recovery.
Compared to foveomacular retinitis, the visual outcome is reported to be better
in cases of solar retinopathy. Abdellah et al[30]
reported that 9 (90%) of 10 eyes had a final visual acuity of 20/25 or more.
Rai et al[3] reported that visual acuity
was 6/12 or better in more than 80% of patients and did not deteriorate in 319
patients. Recent reports have also shown mild to moderate visual loss ranged
from 20/25 to 20/200 in solar
retinopathy[8,11].
In conclusion, foveomacular
retinitis can cause serious visual impairment in young male soldiers. Although
the etiology and risk factors have not yet been established, it is an important
disease to be suspected in cases of sudden or insidious unilateral visual loss
in young soldiers. SD-OCT and fundus IR imaging are required for proper
diagnosis. Further research to elucidate the etiology is needed to prevent
vision loss from this little-known disease.
ACKNOWLEDGEMENTS
Foundations: Supported by the National Research
Foundation of Korea (No.2016R1D1A1B03934724)
funded by the Korean government (Ministry of Science, ICT and Future Planning;
MSIP); Seoul National University Bundang Hospital (No.02-2017-059).
Conflicts of Interest: Yoon CK, None; Park KH, None; Woo
SJ, None.
REFERENCES
|
1 Kuming BS. Foveomacular retinitis. Br J Ophthalmol
1986;70(11): 816-818.
https://doi.org/10.1136/bjo.70.11.816
PMid:3790482 PMCid:PMC1040834
|
|
|
|
2 Agarwal A. Gass' Atlas of Macular Diseases, 5th
Edition. 2012.
|
|
|
|
|
3 Rai N, Thuladar L, Brandt F, Arden GB, Berninger TA.
Solar retinopathy. A study from Nepal and from Germany. Doc Ophthalmol
1998;95(2):99-108.
https://doi.org/10.1023/A:1001160413794
PMid:10431794
|
|
|
|
|
4 Tabatabaei SA, Soleimani M, Bohrani B, Banafsheafshan
A, Faghihi S, Faghihi H. Multimodal imaging in photic retinopathy. Int J
Ophthalmol 2019;12(3):523-525.
|
|
|
|
|
5 Topouzis F, Koskosas A, Pappas T, Anastasopoulos E,
Raptou A, Psilas K. Foveomacular retinitis and associated optical coherence
tomography findings. Ophthalmic Surg Lasers Imaging 2007;38(4):333-335.
https://doi.org/10.3928/15428877-20070701-12
PMid:17674927
|
|
|
|
|
6 Badhani A, Padhi TR, Panda GK, Mukherjee S, Das T,
Jalali S. Correlation of macular structure and function in a boy with primary
foveomacular retinitis and sequence of changes over 5 years. Doc Ophthalmol
2017;135(1):43-52.
https://doi.org/10.1007/s10633-017-9590-1
PMid:28451988
|
|
|
|
|
7 Bechmann M, Ehrt O, Thiel MJ, Kristin N, Ulbig MW,
Kampik A. Optical coherence tomography findings in early solar retinopathy.
Br J Ophthalmol 2000;84(5):547-548.
https://doi.org/10.1136/bjo.84.5.546b
PMid:10847708 PMCid:PMC1723486
|
|
|
|
|
8 Merino-Suárez ML, Belmonte-Martin J, Rodrigo-Auría F,
Pérez-Cambrodí RJ, Piñero DP. Optical coherence tomography and
autofluoresceingraphy changes in solar retinopathy. Can J Ophthalmol
2017;52(2):e67-e71.
https://doi.org/10.1016/j.jcjo.2016.10.010
PMid:28457308
|
|
|
|
|
9 Bonyadi MHJ, Soheilian R, Soheilian M, Peyman GA.
Spectral-domain optical coherence tomography features of mild and severe
acute solar retinopathy. Ophthalmic Surg Lasers Imaging 2011;42.
Online:e84-e86
https://doi.org/10.3928/15428877-20110901-05
PMid:21899248
|
|
|
|
|
10 Birdsong O, Ling J, El-Annan J. Solar retinopathy.
Ophthalmology 2016;123(3):570.
https://doi.org/10.1016/j.ophtha.2016.01.003
PMid:26902564
|
|
|
|
|
11 Gulkilik G, Taskapili M, Kocabora S, Demirci G,
Muftuoglu GI. Association between visual acuity loss and optical coherence
tomography findings in patients with late solar retinopathy. Retina
2009;29(2):257-261.
https://doi.org/10.1097/IAE.0b013e31818a2105
PMid:19033886
|
|
|
|
|
12 Goduni L, Mehta N, Tsui E, Bottini A, Kaden TR,
Leong BCS, Dedania V, Lee GD, Freund KB, Modi YS. Long-term multimodal
imaging of solar retinopathy. Ophthalmic Surg Lasers Imaging Retina 2019;50(6):388-392.
https://doi.org/10.3928/23258160-20190605-08
PMid:31233157
|
|
|
|
|
13 Comander J, Gardiner M, Loewenstein J. High-resolution
optical coherence tomography findings in solar maculopathy and the
differential diagnosis of outer retinal holes. Am J Ophthalmol
2011;152(3):413-419.e6.
https://doi.org/10.1016/j.ajo.2011.02.012
PMid:21708377
|
|
|
|
|
14 Cho HJ, Yoo ES, Kim CG, Kim JW. Comparison of
spectral-domain and time-domain optical coherence tomography in solar
retinopathy. Korean J Ophthalmol 2011;25(4):278-281.
https://doi.org/10.3341/kjo.2011.25.4.278
PMid:21860577 PMCid:PMC3149141
|
|
|
|
|
15 Parodi MB, Casalino G, Iacono P, Introini U, Adamyan
T, Bandello F. The expanding clinical spectrum of choroidal excavation in
macular dystrophies. Retina 2018;38(10):2030-2034.
https://doi.org/10.1097/IAE.0000000000001805
PMid:28800018
|
|
|
|
|
16 Kim H, Woo SJ, Kim YK, Lee SC, Lee CS. Focal
choroidal excavation in multifocal choroiditis and punctate inner
choroidopathy. Ophthalmology 2015;122(7):1534-1535.
https://doi.org/10.1016/j.ophtha.2015.01.012
PMid:25687028
|
|
|
|
|
17 Lee CS, Woo SJ, Kim YK, Hwang DJ, Kang HM, Kim H,
Lee SC. Clinical and spectral-domain optical coherence tomography findings in
patients with focal choroidal excavation. Ophthalmology
2014;121(5):1029-1035.
https://doi.org/10.1016/j.ophtha.2013.11.043
PMid:24439757
|
|
|
|
|
18 Issa PC, Fleckenstein M, Scholl HPN, Holz FG, Meyer
CH. Confocal scanning laser ophthalmoscopy findings in chronic solar
retinopathy. Ophthalmic Surg Lasers Imaging 2008;39(6):497-499.
https://doi.org/10.3928/15428877-20081101-04
PMid:19065982
|
|
|
|
|
19 Ahn SJ, Ahn J, Park KH, Woo SJ. Multimodal imaging
of occult macular dystrophy. JAMA Ophthalmol 2013;131(7):880-890.
https://doi.org/10.1001/jamaophthalmol.2013.172
PMid:24010148
|
|
|
|
|
20 Kerr LM, Little HL. Foveomacular retinitis. Arch
Ophthalmol 1966;76(4):498-504.
https://doi.org/10.1001/archopht.1966.03850010500007
PMid:5928138
|
|
|
|
|
21 Marlor RL, Blais BR, Preston FR, Boyden DG.
Foveomacular retinitis, an important problem in military medicine:
epidemiology. Invest Ophthalmol 1973;12(1):5-16.
|
|
|
|
|
22 Pokroy R, Barenboim E, Carter D, Assa A, Alhalel A.
Unilateral optic disc swelling in a fighter pilot. Aviat Space Environ Med
2009;80(10): 894-897.
https://doi.org/10.3357/ASEM.2341.2009
PMid:19817243
|
|
|
|
|
23 Mumcuoglu T, Durukan AH, Erdurman C, Hurmeric V,
Karagul S. Outcomes of Nd: YAG laser treatment for Valsalva retinopathy due
to intense military exercise. Ophthalmic Surg Lasers Imaging
2009;40(1):19-24.
https://doi.org/10.3928/15428877-20090101-15
PMid:19205491
|
|
|
|
|
24 Blanch RJ, Bindra MS, Jacks AS, Scott RA. Ophthalmic
injuries in British armed forces in Iraq and Afghanistan. Eye (Lond)
2011;25(2):218-223.
https://doi.org/10.1038/eye.2010.190
PMid:21164529 PMCid:PMC3169213
|
|
|
|
|
25 Yannuzzi LA, Jampol LM, Rabb MF, Sorenson JA, Beyrer
C, Wilcox LM Jr. Unilateral acute idiopathic maculopathy. Arch Ophthalmol
1991;109(10):1411-1416.
https://doi.org/10.1001/archopht.1991.01080100091049
PMid:1929931
|
|
|
|
|
26 Nicolo M, Rosa R, Musetti D, Musolino M, Traverso
CE. Early swept-source optical coherence tomography angiography findings in
unilateral acute idiopathic maculopathy. Ophthalmic Surg Lasers Imaging
Retina 2016;47(2):180-182.
https://doi.org/10.3928/23258160-20160126-13
PMid:26878453
|
|
|
|
|
27 Matsushita E, Fukuda K, Nakahira A, Kishi S,
Fukushima A. Resolution of photoreceptor outer segment damage in a patient
with unilateral acute idiopathic maculopathy observed using spectral-domain
optical coherence tomography. Graefes Arch Clin Exp Ophthalmol
2012;250(5):765-768.
https://doi.org/10.1007/s00417-011-1796-4
PMid:22261750
|
|
|
|
|
28 Iu LPL, Lee R, Fan MCY, Lam WC, Chang RT, Wong IYH.
Serial spectral-domain optical coherence tomography findings in acute retinal
pigment epitheliitis and the correlation to visual acuity. Ophthalmology
2017;124(6):903-909.
https://doi.org/10.1016/j.ophtha.2017.01.043
PMid:28284786
|
|
|
|
|
29 Cho HJ, Han SY, Cho SW, Lee DW, Lee TG, Kim CG, Kim
JW. Acute retinal pigment epitheliitis: spectral-domain optical coherence
tomography findings in 18 cases. Invest Ophthalmol Vis Sci
2014;55(5):3314-3319.
https://doi.org/10.1167/iovs.14-14324
PMid:24787563
|
|
|
|
|
30 Abdellah MM, Mostafa EM, Anber MA, El Saman IS,
Eldawla ME. Solar maculopathy: prognosis over one year follow up. BMC
Ophthalmol 2019;19(1):201.
https://doi.org/10.1186/s12886-019-1199-6
PMid:31533669 PMCid:PMC6749640
|
|