·Meta-Analysis·
Vitrectomy
with internal limiting membrane peeling versus its flap insertion for macular
hole in high myopia: a Meta-analysis
Ya-Jun
Wu1, Jie Rao1, Kang-Rui Wu1, Na Wu1,
Yi Cheng1, Xiao-Xuan Xu1, Li Yan1, Yi Shao1,
Yu Tian2, Xiao-Rong Wu1
1Department of Ophthalmology, the
First Affiliated Hospital of Nanchang University, Nanchang 330006, Jiangxi
Province, China
2Department of Ophthalmology, the
Second Xiangya Hospital, Central South University, Changsha 410008, Hunan
Province, China
Co-first authors: Ya-Jun Wu and Jie Rao
Correspondence to: Xiao-Rong Wu. Department of
Ophthalmology, the First Affiliated Hospital of Nanchang University, Nanchang
330006, Jiangxi Province, China. wxr98021@126.com; Yu Tian. Department of
Ophthalmology, the Second Xiangya Hospital, Central South University, Changsha
410008, Hunan Province, China. tianyu3734358@csu.edu.cn
Received: 2019-05-19
Accepted: 2019-07-23
Abstract
AIM: To compare the
anatomic and functional outcomes between vitrectomy with internal limiting
membrane (ILM) peeling and internal ILM flap insertion technique for high
myopia macular hole (MH).
METHODS: PubMed, Cochrane
Library, EMBASE, and CNKI were systematically searched, and all studies
involved MH were included. The closure rate of MH and the postoperative
best-corrected visual acuity (BCVA) at 6mo after the initial surgery were the
primary measures. All statistical tests were performed in Review Manager 5.3.
RESULTS: Five studies that
included 151 eyes of 151 patients were finally included, all of which were
retrospectively comparative studies. Between the pars plana vitrectomy (PPV)
with ILM peeling surgery and the ILM insertion technique, the latter had
significantly better efficacy with respect to the closure rate of MH (OR=21.32,
95%CI=7.25-62.67, P<0.001); However, regarding BCVA at 6mo after the
initial surgery in MH, there was no statistical significance between the groups
(OR=-0.04, 95%CI=-0.22-0.14, P=0.66). In addition, regarding the rate of
retinal reattachment after the initial surgery, the two different methods were
not significantly different (OR=2.22, 95%CI=0.34-14.32, P=0.4).
CONCLUSION: Both ILM peeling and
ILM insertion technique could significantly improve anatomic outcomes of MH in
high myopia with or without retinal detachment (RD), and anatomic outcomes are
more effective. However, there is no statistical significance in BCVA at 6mo
after the initial surgery in MH, or in the rate of retinal reattachment after
the first surgery, between the two methods.
KEYWORDS: macular hole; high
myopia; best-corrected visual acuity; retinal
attachment; Meta-analysis
DOI:10.18240/ijo.2020.01.21
Citation:
Wu YJ, Rao J, Wu KR, Wu N, Cheng Y, Xu XX, Yan L, Shao Y, Tian Y, Wu XR.
Vitrectomy with internal limiting membrane peeling versus its flap insertion
for macular hole in high myopia: a Meta-analysis. Int J Ophthalmol
2020;13(1):141-148
INTRODUCTION
Macular hole (MH) is a
full-thickness neuroretinal defect that occurs in the retina. According to the
International Vitreomacular Traction Study (IVTS), vitreous liquefaction will
lead to posterior vitreous detachment and further progress to vitreous macular
adhesion, which can eventually develop into pathological vitreous macular
traction and MH, the latter usually will result in the damage to central
vision. High myopia MH [axial length >26 mm
or diopter (D) of at least 6[1]] is one of the
most common types of MH, which can easily lead to retinal detachment (RD)[2-3].
Vitrectomy with traditional internal
limiting membrane (ILM) peeling technique is regarded as the gold standard
treatment for MH; it works by completely relieving of the traction of the
macula and increasing the flexibility of the retina[4].
However, the ILM peeling technique may fail to close the hole, or may cause
secondary MH or foveoschisis[5-6].
Recently, an ILM insertion technique was developed; it has steadily grown in
popularity as a modified method for treatment of high myopia MH. In fact, there
are several different inverted ILM flap techniques, among them. Free ILM flap
and inverted ILM flaps are most commonly used in the surgery. Morizane et al[7] first reported the ILM insertion technique; they
transplanted the free ILM to fill the hole, and confirmed that the insertion
technique was an effective approach for persistent refractory MHs, including in
patients with high myopia MHs that did not close after conventional ILM peeling
approach. In order to improve the cure rate of MH, Chen and Yang[8] attempted to peel part of the ILM along the edge of the
hole, taking care not to remove it completely, and then inverted the ILM and
inserted it into the hole. Eventually they confirmed that compared to ILM
peeling alone, the inverted ILM insertion technique could help improve the rate
of closure of high myopia MHs.
However, there have not been large
numbers of investigations to distinguish the outcomes such as the MH closure
rate between conventional pars plana vitrectomy (PPV) combined with ILM peeling
and PPV combined with ILM insertion into the MH. Thus, in order to determine
which approach has better anatomic and functional outcomes after the initial
operation, we performed a Meta-analysis to compare these two methods for the
treatment of high myopia MH. We assessed MH closure rate and best-corrected
visual acuity (BCVA) at 6mo after the initial surgery, as well as the rate of
retinal reattachment in patients with high myopia MH combined with RD.
MATERIALS AND METHODS
This Meta-analysis was conducted
according to the Preferred Reporting Items for Systematic Reviews and
Meta-Analyses (PRISMA) guidelines.
Search Strategy In this Meta-analysis, all relevant
studies were hunted from PubMed, Cochrane Library, Embase and CKNI (the largest
database of science in China). We were searching the studies by using following
terms: “macular hole” OR “retinal break” AND “high myopia” AND “internal
limiting membrane peeling” OR “ILM flap insertion”. Final search was carried
out on June 2018. There were no restrictions in included articles’ language and
publishing year. Studies with available dates were included. Review, case
report, meeting abstract and articles lacks comparing were excluded.
Criteria For Inclusion and Exclusion
Data inclusion The considering studies should
fulfill following criteria: 1) comparing outcomes of patients treated with
vitrectomy with conventional ILM peeling vs ILM flap insertion for MH in
high myopia; 2) retrospective study reported the surgery treatment for MH in
high myopia; 3) reporting the detailed and sufficient outcomes, such as the
rate of MH closure and BCVA, and following-up’s data.
By reading titles and abstracts, two
independent investigators (Yan L and Wu N) roughly selected useful articles,
also they read the full texts to choose those potential literatures in the
Meta-analysis, which following above criteria.
Data extraction Two reviewers extracted information
from included studies independently and rechecked carefully. Any disagreement
regarding eligibility during the extraction was discussed by the two reviewers
and had been resolved. The data from selected studies included the first
author, publication year, country, trial type, age, gender, axial length number
of subjects, surgical procedures, gas used, closure rate preoperative and
postoperative BCVA. The exclusive criteria as follows: 1) the study was
designed “as reviews but without primary outcomes” or “case reports” or
“meeting abstracts”; 2) the study was prospective multicenter randomized
controlled trial (RCT); 3) the research objects were animals rather than human;
4) the operative date was poor or unavailable in the literatures. In order to
get high-quality studies, two independent reviewers participated in excluding
articles following above criteria.
Statistical Analysis Cochrane Collaboration’s Review
Manager Software (RevMan Version 5.3, Cochrane Community) was used for data
analysis. We analyzed dichotomous variables: the closure rate of MH by using
estimation of odds ratios (OR) with a 95% confidence interval (CI). For
continuous outcome data like BCVA, we converted these data to the mean and
standard deviation by using the method reported by Hozo et al[9]. Statistical heterogeneity among studies was evaluated
with the Q test and I2 statistic, and P<0.1
and I2>50% indicating significant heterogeneity. If P<0.1
and I2>50%, a random-effects model was used for the
Meta-analysis; otherwise, the fixed-effect model was used. Publication bias was
evaluated by using a funnel plot.
RESULTS
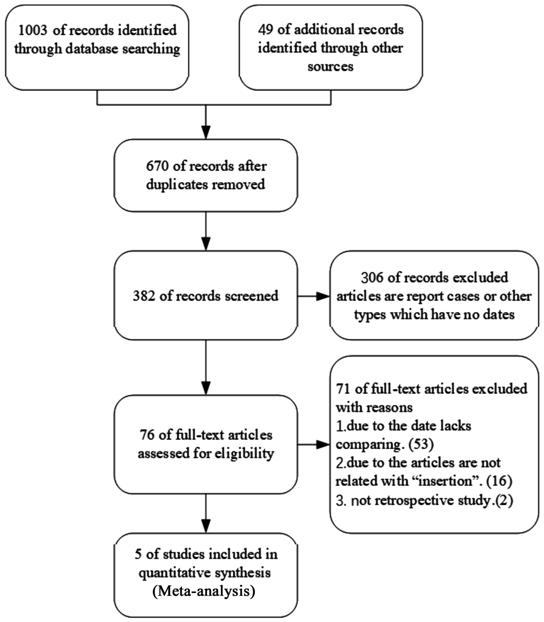
Selection of Studies In total, 1052 articles were
initially identified; 1003 of these were identified in database searches, while
49 records were found through other sources. After removal of duplicate
records, 670 studies were retained; following application of the inclusion and
exclusion criteria, 5 articles, which were all retrospective studies, were used
in this analysis[8,10-13].
The process is illustrated in greater detail in the flow diagram of Figure 1.
Figure 1 Flow diagram of the
literature search strategy.
Characteristics and Baseline of the
Included Studies This Meta-analysis included 5
studies, which involved 151 eyes; 62 eyes underwent ILM flap insertion, while
89 eyes underwent conventional ILM peeling. The characteristics of these eyes
are listed in Table 1, including age, sex, presence or absence of RD, and axial
length. Intraoperative staining of the ILM was performed by indocyanine green
(ICG), brilliant blue G (BBG) or triamcinolone acetonide (TA); gas tamponade
involving sulfur hexafluoride (SF6) or perfluoropropane (C3F8), and silicone
oil (SO) was used after ILM peeling.
All studies were retrospective
analyses; two were performed in Japan, three in Taiwan, China (Table 1). Table
2 depicts the quality of studies included in this Meta-analysis; total scores
ranged from 14 to 18, generally speaking, the quality of researches were
moderate to good.
Table 2 MINORS for assessing quality
of included studies
|
Methodological item for
non-randomized studies
|
Chen et al[8],
2016
|
Baba et al[10],
2017
|
Wu et al[11],
2017
|
Wakabayashi et al[12],
2018
|
Chen et al[13],
2018
|
|
1. A clearly stated aim
|
2
|
2
|
2
|
2
|
2
|
|
2. Inclusion of consecutive
patients
|
2
|
2
|
2
|
2
|
2
|
|
3. Prospective collection of data
|
2
|
0
|
1
|
2
|
2
|
|
4. Endpoints appropriate to the
aim of the study
|
2
|
2
|
2
|
2
|
2
|
|
5. Unbiased assessment of the
study endpoint
|
0
|
0
|
0
|
0
|
0
|
|
6. Follow-up period appropriate to
the aim of the study
|
2
|
2
|
2
|
0
|
2
|
|
7. Loss to follow up less than 5%
|
2
|
2
|
2
|
2
|
2
|
|
8. Prospective calculation of the
study size
|
0
|
0
|
0
|
0
|
0
|
|
9. An adequate control group
|
2
|
2
|
2
|
2
|
2
|
|
10. Contemporary groups
|
0
|
0
|
0
|
0
|
0
|
|
11. Baseline equivalence of groups
|
2
|
2
|
2
|
0
|
2
|
|
12. Adequate statistical analyses
|
2
|
2
|
2
|
2
|
2
|
|
Total score
|
18
|
16
|
17
|
14
|
18
|
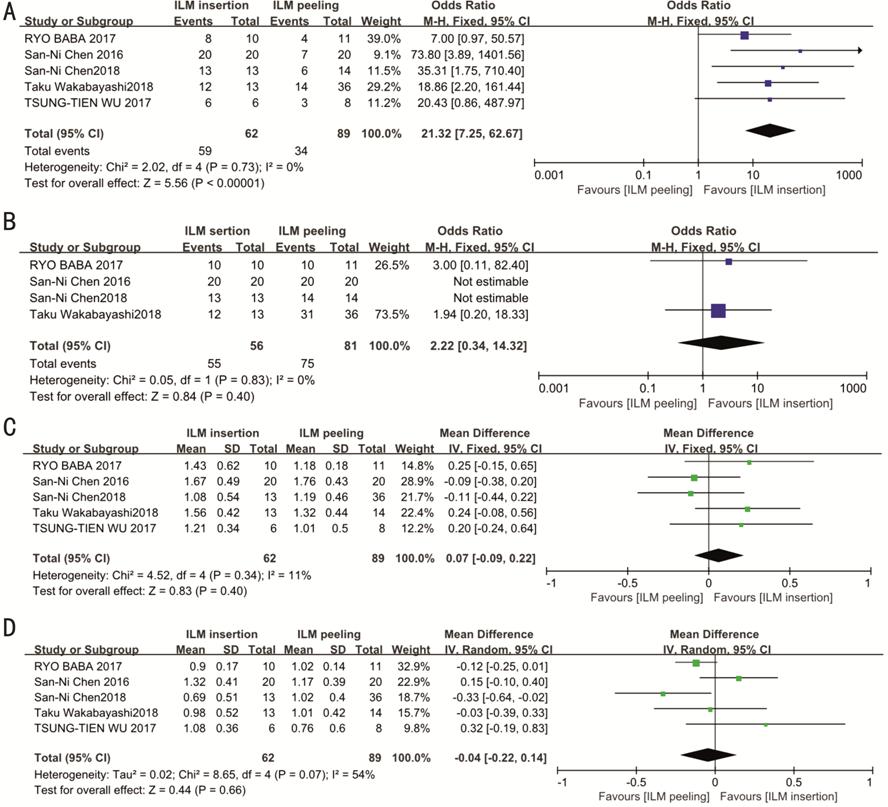
Outcomes of the Meta-analysis Figure 2 shows forest plots
comparing the results of the ILM insertion group with those of the ILM peeling
group; the rate of closure of MH in the ILM insertion group was significantly
better than that of the ILM peeling group in all studies (OR=21.32,
95%CI=7.25-62.67, P<0.001, Figure 2A), with no heterogeneity (I2=0,
P=0.73, Figure 2A). In
the subgroup Meta-analysis of patients with MH combined with RD, 4 studies were
finally included; there was no significant difference in the rate of retinal
reattachment of the MH between the ILM insertion and ILM peeling groups
(OR=2.22, 95%CI=0.34-14.32, P=0.4, Figure 2B); no heterogeneity was
detected (I2=0, P=0.83, Figure 2B). In order to
determine which method could more clearly improve BCVA, we constructed two
subgroups, preoperative BCVA and postoperative BCVA (6mo after the initial
surgery); we used these groups to compare the effect between the conventional
surgery and the insertion technique. The Figure 2 shows that preoperative BCVA
was recorded in all 5 studies; there was no statistically significant
difference between the techniques (OR=0.07, 95%CI=-0.09-0.22, P=0.4,
Figure 2C). The postoperative
BCVA also showed no significant difference between the ILM insertion and ILM
peeling groups (OR= -0.04, 95%CI=-0.22-0.14, P=0.66, Figure 2D); both
subgroups exhibited heterogeneity (preoperative group, I2=11%,
P=0.34, Figure 2C;
postoperative group, I2=54%, P=0.07, Figure 2D).
Because the postoperative group showed high heterogeneity (I2>50%),
a random model was used.
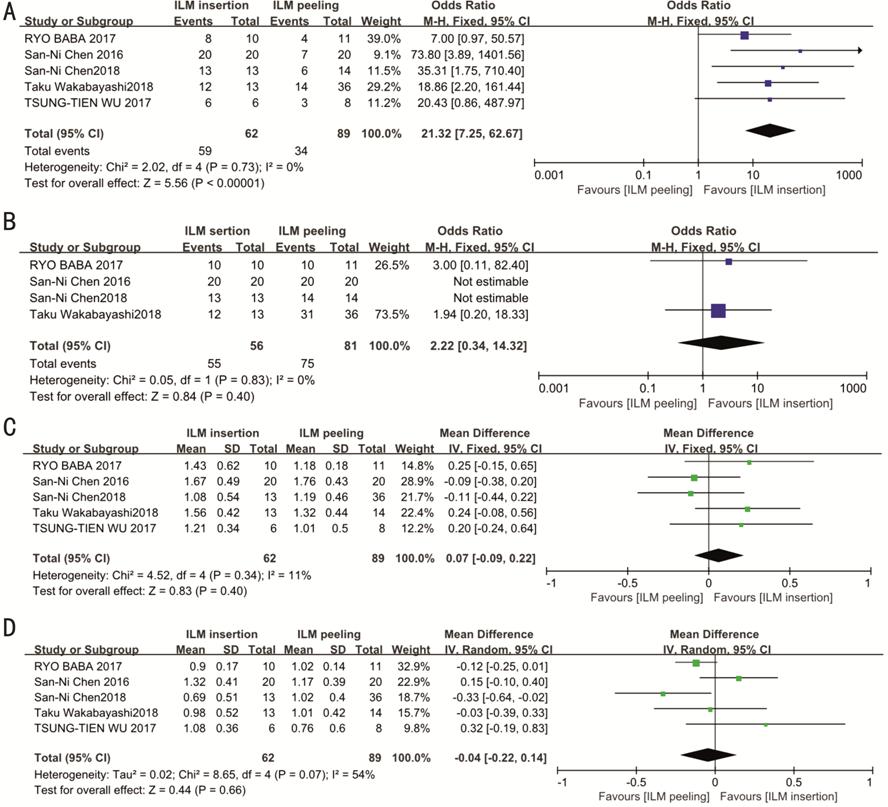
Figure 2 Forest plots of anatomic
and functional outcomes of MH in high myopia after the first surgery A: The closure rate of MH of the all 5
studies; B: The retinal reattachment of MH of patients with RD; C: Preoperative
BCVA of the all 5 studies; D: Postoperative BCVA later 6mo after the first
surgery.
Additionally, in the subgroup of MH
combined with RD, due to the cumulative effect, two articles were excluded by
Review manager 5.3[8,13]; their
rates of retinal reattachment in MH were 100% in both the ILM insertion and ILM
peeling groups, such that ORs could not be calculated.
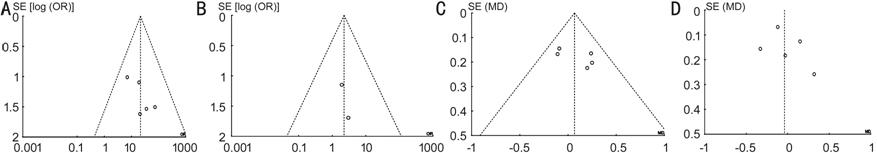
Testing for Publication Bias Figure 3 shows all four funnel plots
for the closure rate, preoperative and postoperative BCVA, and retinal
reattachment; none of these data exhibited obvious asymmetries, indicating that
there was no serious publication bias in the included studies.
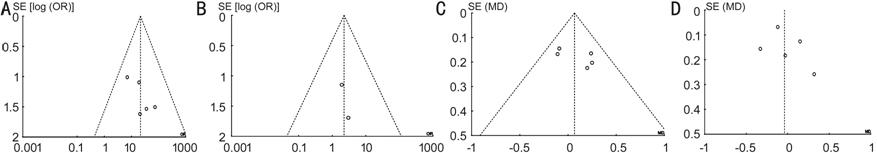
Figure 3 Funnel plots of literatures
included in this Meta-analysis A: The
closure rate of MH of the all 5 studies; B: The retinal reattachment of MH of
patients with RD; C: Preoperative BCVA of the all 5 studies; D: Postoperative
BCVA later 6mo after the first surgery.
DISCUSSION
In this Meta-analysis, we included 5
studies that all compared the effects of the methods for surgical treatment of
high myopia MH between the conventional ILM peeling technique and the modified
ILM insertion technique. In total, 151 eyes of 151 patients were evaluated
regarding the postoperative closure rate of the hole, which is the most
critical ophthalmic examination result; moreover, we evaluated the preoperative
and postoperative BCVA (6mo after the initial surgery). Additionally, we
performed subgroup analysis regarding the rate of retinal reattachment after
the initial surgery, among patients who exhibited MH combined with RD, which
included the data from 4 studies. Many studies of ILM insertion have reported[8,10-13] that the
ILM insertion technique could improve the closure rate, compared with that of
conventional PPV with ILM peeling. In cases where the hole remained open after
the initial operation, surgeons could choose to use the ILM flap to fill the
hole; for treatment of recurrent and chronic patients, this modified technique
could help to close the hole and to improve visual function[14].
In our study, the forest plot revealed that the insertion technique was better
(P<0.05). However, regarding the rate of retinal reattachment after
the initial surgery and the postoperative BCVA, there were no significant
differences (P>0.05); the subgroup with high myopia MH with RD, a
small amount of eyes were included, which may have led to the results of the
forest plot (P>0.05).
Kelly and Wendel[15]
first reported operative treatment for MH, which comprised PPV. Before
that report, MH was considered incurable; Yooh et al[16]
then demonstrated that ILM peeling combined with PPV was more effective for
treatment of MH. Recently, this surgical method has been used for high myopia
MH, with or without RD[17-19].
The surgical procedures have become standardized; thus, after the completion of
PPV, experienced surgeons would use dye to identify the ILM, which was then
peeled carefully in a circular manner around the hole by use of an ILM forceps,
and completely removed from the retina. After fluid-gas exchange (injection of
perfluoropropane gas tamponade or other gas into the vitreous cavity), patients
were instructed to remain in the face-down position for approximately 2wk
postoperatively; then, ophthalmic examination results were checked. Studies
have shown a good anatomic outcome using simple MH; the approximate
postoperative closure rate could reach 88%[20-21]; despite this considerable success in closure rate,
an unavoidable failing rate could not be ignored, such that the hole may
continue opening after operation. Additionally, for patients with MH combined
with RD, the closure rate varied from 10%-70%[22].
Importantly, the ILM peeling approach often led to poor functional outcomes,
especially with regard to postoperative visual outcomes[23-24]; some complications, such as outer retinal cysts,
appeared after surgery because of leaking tissue in the subfoveal area[23].
In order to resolve patients’
frustrations, reduce complications, and improve the success rate of the
operations, many operators attempted to modify surgical processes, which were
based on the traditional standard surgery method. In 2010, Michalewska et al[25] first reported the inverted ILM technique; they
speculated that this modified technique could improve both anatomic and
functional outcomes. The process of PPV was identical to that of the
conventional technique. With respect to the ILM, Michalewska et al[25] peeled it around the hole for approximately 2
disc diameters; then, instead of completely removing the peeled ILM, they
maintained a few fringes of ILM that were attached to the edge of the hole. In
the next step, the ILM was inverted sufficiently to cover the surface of the
hole; in this manner, glial cells might proliferate and then fill in the hole,
resulting in ultimate closure of the hole. Furthermore, the ILM insertion
technique was also a modified technique, similar to the classic inverted
method; the primary difference was the processing procedure used for the ILM,
such that the ILM was used to fill the hole, rather than to cover it. The
Japanese ophthalmologists, Chen et al[8,13] performed multiple investigations of the insertion
technique; in another study, they used the free ILM flap to treat chronic and
persistent MH. After some effective surgeries, they found that, in patients who
had MH combined with RD, the insertion technique had a higher closure rate than
the conventional ILM peeling technique; moreover, insertion of double ILM could
fix it well into the hole. Furthermore, many other ophthalmologists used the
inverted ILM flap to fill and close the hole[6,21,26-28]. However,
the submacular retinal pigment epithelium (RPE) exhibited atrophy 1wk after
insertion of the ILM flap into the hole. Imai and Azumi[26]
speculated that the insertion technique may cause this condition. Fortunately,
Chen and Yang[8] determined that the dye agent,
ICG, was the source of the atrophy; clinicians should rinse away the ICG as
soon as possible, because the toxicity of ICG may cause RPE atrophy. In
contrast, change other safe one like BBG was better.
Notably, simply covering the surface
of hole with ILM was worse than filling it[29],
especially when the hole was particularly large or persisted postoperatively.
Many studies have reported that the insertion technique has better anatomic and
functional outcomes[13,30].
According to the study by Park et al[29]
in some complex types of MH, such as big MH and high myopia MH, the insertion
technique showed better recovery of the photoreceptor layers, compared with the
classic inverted technique; moreover, the insertion technique also exhibited
better visual outcome after surgery. Baba et al[10]
believed that keeping the glial cells in the hole during surgery may facilitate
the closure of the hole for high myopia MH. Rossi et al[31] investigated speculated that using the ILM flap to
fill the hole could improve the closure rate more effectively than the classic
inverted technique.
Importantly, the insertion technique
has some advantages that are absent from the inverted covering technique.
Previously, there was a Meta-analysis comparing the conventional peeling
technique with the inverted technique by Yuan et al[32]; they showed that the inverted technique had a better
effect on the closure rate at 6mo after the initial surgery, compared with the
conventional technique; however, it did not result in better visual outcomes.
The current insertion technique has thus far lacked a systematic comparison
with the conventional gold standard technique. Yet, some interesting
literatures have filled this gap. Currently, the ILM, which is used to fill the
hole, has two types of ILM insertion technique, free ILM flap or inverted ILM
flap. Of course, the latter approach was modified on the basis of the inverted
covering technique. Zheng et al[33]
randomly distributed 38 patients with high myopia MH into two groups; group 1
used the conventional PPV with ILM peeling technique, group 2 used the inverted
ILM insertion technique. They found that the patients in group 2 had fewer
complications and a better closure rate at 3mo after the initial surgery.
Moreover, the insertion technique was concluded to be more effective and safer.
Chen et al[13] used the free ILM flap,
inserted into the hole of high myopia MH patients; after the operations, they
found that this new technique had a higher closure rate than ILM peeling.
However, in a recent study, Velez‑Montoya et al[34]
also used free ILM flap to fill the hole, and compared their findings
with the postoperative effect of conventional ILM peeling. Notably, regarding
the postoperative closure rate, that of the free flap technique was
approximately 85% less than that of the conventional ILM peeling technique
(91%); they speculated that the small number of patients may have contributed
to this unusual finding.
In order to eliminate disputes, in
this Meta-analysis, we searched studies comparing the ILM peeling and ILM
insertion techniques. We systematically compared the anatomic and functional
outcomes between these two techniques for patients with high myopia MH after
the initial surgery, in order to ensure that this new modified technique would
improve both anatomic and functional outcomes. We found 5 studies that
concluded the ILM insertion technique could improve both closure rate and
visual condition; among these 5 studies, 4[8,10,12-13] included
patients with RD, and showed that the rate of retinal reattachment was higher
when using the insertion technique. After statistical analysis, we concluded
that the insertion technique was the better choice, as it can provide a higher
closure rate; however, the postoperative BCVA at 6mo after surgery was not
statistically different between the two methods. We suspect that this may be
due to the small number of patients. The deficiencies in our study were the
limited data available to analyze retinal reattachment between the two groups.
Notably, of the 4 studies that included patients with high myopia MH combined
with RD, the patients all exhibited retinal reattachment after surgery in ILM
peeling and ILM insertion technique; we could not find a statistical difference
between the two groups.
These results are representative and
rigorous; surgeons may consider that, for patients with high myopia MH, the ILM
insertion technique is a better method for hole closure.
The ILM insertion technique had
better anatomical outcome with regard to closure rate for patients with high
myopia MH, with or without RD; however, functional outcomes, such as BCVA or
retinal reattachment, were similar to those of traditional ILM peeling.
Additional studies with more patients may be needed to confirm these findings.
ACKNOWLEDGEMENTS
Foundations: Supported by National Natural
Science Foundation of China (No.81760179, No.81360151); Natural Science
Foundation of Jiangxi Province (No.20171BAB205046); Key Foundation of Education
Department of Jiangxi Province (No.GJJ160033); Health Development Planning
Commission Science Foundation of Jiangxi Province (No.20185118); Foundation of
Science and Technology Supported by Jiangxi Province (No.20141BBG70027);
Chinese Medicine Research Project of Jiangxi Health and Family Planning
Commission (No.2017A001);
Jiangxi Province Grass-Roots Health Appropriate Technology Spark Promotion
Project (No.20188007); Jiangxi Provincial Health and FP General Plan
(No.20141031); General Project of Jiangxi Provincial Education Department
(No.GJJ13147).
Conflicts of Interest: Wu YJ, None; Rao J, None; Wu KR, None;
Wu N, None; Cheng Y, None; Xu XX, None; Yan L,
None; Shao Y, None; Tian Y, None; Wu XR, None.
REFERENCES
|
1 Young TL, Ronan SM, Drahozal LA, Wildenberg
SC, Alvear AB, Oetting WS, Atwood LD, Wilkin DJ, King RA. Evidence that a
locus for familial high myopia maps to chromosome 18p. Am J Hum Genet
1998;63(1):109-119.
https://doi.org/10.1086/301907
PMid:9634508 PMCid:PMC1377231
|
|
|
|
2 Margheria RR, Schepens CL. Macular
breaks. 1. Diagnosis, etiology, and observations. Am J Ophthalmol
1972;74(2):219-232.
https://doi.org/10.1016/0002-9394(72)90537-5
|
|
|
|
|
3 Panozzo G, Mercanti A. Optical coherence
tomography findings in myopic traction maculopathy. Arch Ophthalmol
2004;122(10):1455-1460.
https://doi.org/10.1001/archopht.122.10.1455
PMid:15477456
|
|
|
|
|
4 Sayanagi K, Ikuno Y, Tano Y. Tractional
internal limiting membrane detachment in highly myopic eyes. Am J Ophthalmol
2006;142(5): 850-852.
https://doi.org/10.1016/j.ajo.2006.05.031
PMid:17056366
|
|
|
|
|
5 Ho TC, Chen MS, Huang JS, Shih YF, Ho H,
Huang YH. Foveola nonpeeling technique in internal limiting membrane peeling of
myopic foveoschisis surgery. Retina 2012;32(3):631-634.
https://doi.org/10.1097/IAE.0b013e31824d0a4b
PMid:22374159
|
|
|
|
|
6 Kuriyama S, Hayashi H, Jingami Y, Kuramoto
N, Akita J, Matsumoto M. Efficacy of inverted internal limiting membrane flap
technique for the treatment of macular hole in high myopia. Am J Ophthalmol
2013;156(1):125-131.e1.
https://doi.org/10.1016/j.ajo.2013.02.014
PMid:23622567
|
|
|
|
|
7 Morizane Y, Shiraga F, Kimura S, Hosokawa
M, Shiode Y, Kawata T, Hosogi M, Shirakata Y, Okanouchi T. Autologous
transplantation of the internal limiting membrane for refractory macular holes.
Am J Ophthalmol 2014;157(4):861-869.e1.
https://doi.org/10.1016/j.ajo.2013.12.028
PMid:24418265
|
|
|
|
|
8 Chen SN, Yang CM. Inverted internal
limiting membrane insertion for macular hole-associated retinal detachment in
high myopia. Am J Ophthalmol 2016;162:99-106.el.
https://doi.org/10.1016/j.ajo.2015.11.013
PMid:26582311
|
|
|
|
|
9 Hozo SP, Djulbegovic B, Hozo I.
Estimating the mean and variance from the median, range, and the size of a
sample. BMC Med Res Methodol 2005;5:13.
https://doi.org/10.1186/1471-2288-5-13
PMid:15840177 PMCid:PMC1097734
|
|
|
|
|
10 Baba R, Wakabayashi Y, Umazume K,
Ishikawa T, Yagi H, Muramatsu D, Goto H. Efficacy of the inverted internal
limiting membrane flap technique with vitrectomy for retinal detachment
associated with myopic macular holes. Retina 2017;37(3):466-471.
https://doi.org/10.1097/IAE.0000000000001211
PMid:28225722
|
|
|
|
|
11 Wu TT, Kung YH, Chang CY, Chang SP. Surgical
outcomes in eyes with extremely high myopia for macular hole without retinal
detachment. Retina 2018;38(10):2051-2055.
https://doi.org/10.1097/IAE.0000000000001806
PMid:28796147
|
|
|
|
|
12 Wakabayashi T, Ikuno Y, Shiraki N,
Matsumura N, Sakaguchi H, Nishida K. Inverted internal limiting membrane
insertion versus standard internal limiting membrane peeling for macular hole
retinal detachment in high myopia: one-year study. Graefes Arch Clin Exp
Ophthalmol 2018;256(8):1387-1393.
https://doi.org/10.1007/s00417-018-4046-1
PMid:29911271
|
|
|
|
|
13 Chen SN, Hsieh YT, Yang CM. Multiple free
internal limiting membrane flap insertion in the treatment of macular
hole-associated retinal detachment in high myopia. Ophthalmologica
2018;240(3): 143-149.
https://doi.org/10.1159/000487337
PMid:29874671
|
|
|
|
|
14 Iwakawa Y, Imai H, Kaji H, Mori Y, Ono
C, Otsuka K, Miki A, Oishi M. Autologous transplantation of the internal
limiting membrane for refractory macular hole following ruptured retinal
arterial macroaneurysm: A case report. Case Rep Ophthalmol 2018;9(1):113-119.
https://doi.org/10.1159/000485914
PMid:29643791 PMCid:PMC5892329
|
|
|
|
|
15 Kelly NE, Wendel RT. Vitreous surgery for
idiopathic macular holes. Results of a pilot study. Arch Ophthalmol
1991;109(5):654-659.
https://doi.org/10.1001/archopht.1991.01080050068031
PMid:2025167
|
|
|
|
|
16 Yooh HS, Brooks HL Jr, Capone A Jr,
L'Hernault NL, Grossniklaus HE. Ultrastructural features of tissue removed
during idiopathic macular hole surgery. Am J Ophthalmol 1996;122(1):67-75.
https://doi.org/10.1016/S0002-9394(14)71965-8
|
|
|
|
|
17 García-Arumí J, Martinez V, Puig J,
Corcostegui B. The role of vitreoretinal surgery in the management of myopic
macular hole without retinal detachment. Retina 2001;21(4):332-338.
https://doi.org/10.1097/00006982-200108000-00006
PMid:11508878
|
|
|
|
|
18 Kadonosono K, Yazama F, Itoh N, Uchio E,
Nakamura S, Akura J, Sawada H, Ohno S. Treatment of retinal detachment resulting
from myopic macular hole with internal limiting membrane removal. Am J
Ophthalmol 2001;131(2):203-207.
https://doi.org/10.1016/S0002-9394(00)00728-5
|
|
|
|
|
19 Kuhn F. Internal limiting membrane
removal for macular detachment in highly myopic eyes. Am J Ophthalmol
2003;135(4):547-549.
https://doi.org/10.1016/S0002-9394(02)02057-3
|
|
|
|
|
20 Williamson TH, Lee E. Idiopathic macular
hole: analysis of visual outcomes and the use of indocyanine green or
brilliant blue for internal limiting membrane peel. Graefes Arch Clin Exp
Ophthalmol 2014;252(3):395-400.
https://doi.org/10.1007/s00417-013-2477-2
PMid:24146267
|
|
|
|
|
21 Michalewska Z, Michalewski J,
Dulczewska-Cichecka K, Adelman RA, Nawrocki J. Temporal inverted internal
limiting membrane flap technique Versus Classic Inverted Internal Limiting
Membrane Flap Technique: A Comparative Study. Retina 2015;35(9):1844-1850.
https://doi.org/10.1097/IAE.0000000000000555
PMid:25946691
|
|
|
|
|
22 Oie Y, Emi K, Takaoka G, Ikeda T. Effect
of indocyanine green staining in peeling of internal limiting membrane for
retinal detachment resulting from macular hole in myopic eyes. Ophthalmology
2007;114(2):303-306.
https://doi.org/10.1016/j.ophtha.2006.07.052
PMid:17194478
|
|
|
|
|
23 Michalewska Z, Michalewski J, Cisiecki
S, Adelman R, Nawrocki J. Correlation between foveal structure and visual outcome
following macular hole surgery: a spectral optical coherence tomography
study. Graefes Arch Clin Exp Ophthalmol 2008;246(6):823-830.
https://doi.org/10.1007/s00417-007-0764-5
PMid:18386040
|
|
|
|
|
24 Michalewska Z, Michalewski J, Nawrocki
J. Diagnosis and evaluation of macular hole with the HRT 2 retina module.
Ophthalmologe 2007;104(10):881-888.
https://doi.org/10.1007/s00347-007-1558-1
PMid:17674007
|
|
|
|
|
25 Michalewska Z, Michalewski J, Adelman
RA, Nawrocki J. Inverted internal limiting membrane flap technique for large
macular holes. Ophthalmology 2010;117(10):2018-2025.
https://doi.org/10.1016/j.ophtha.2010.02.011
PMid:20541263
|
|
|
|
|
26 Imai H, Azumi A. The expansion of RPE
atrophy after the inverted ILM flap technique for a chronic large macular hole.
Case Rep Ophthalmol 2014;5(1):83-86.
https://doi.org/10.1159/000360693
PMid:24707278 PMCid:PMC3975172
|
|
|
|
|
27 Shin MK, Park KH, Park SW, Byon IS, Lee
JE. Perfluoro-n-octane-assisted single-layered inverted internal limiting
membrane flap technique for macular hole surgery. Retina
2014;34(9):1905-1910.
https://doi.org/10.1097/IAE.0000000000000339
PMid:25154029
|
|
|
|
|
28 Michalewska Z, Michalewski J,
Dulczewska-Cichecka K, Nawrocki J. Inverted internal limiting membrane flap
technique for surgical repair of myopic macular holes. Retina
2014;34(4):664-669.
https://doi.org/10.1097/IAE.0000000000000042
PMid:24263468
|
|
|
|
|
29 Park JH, Lee SM, Park SW, Lee JE, Byon
IS. Comparative analysis of large macular hole surgery using an internal limiting
membrane insertion versus inverted flap technique. Br J Ophthalmol
2019;103(2):245-250.
https://doi.org/10.1136/bjophthalmol-2017-311770
PMid:29610221
|
|
|
|
|
30 Chen SN, Yang CM. Double internal
limiting membrane insertion for macular hole-associated retinal detachment. J
Ophthalmol 2017;2017:3236516.
https://doi.org/10.1155/2017/3236516
PMid:28845304 PMCid:PMC5560081
|
|
|
|
|
31 Rossi T, Gelso A, Costagliola C, Trillo
C, Costa A, Gesualdo C, Ripandelli G. Macular hole closure patterns
associated with different internal limiting membrane flap techniques. Graefes
Arch Clin Exp Ophthalmol 2017;255(6):1073-1078.
https://doi.org/10.1007/s00417-017-3598-9
PMid:28161828
|
|
|
|
|
32 Yuan J, Zhang LL, Lu YJ, Han MY, Yu AH, Cai
XJ. Vitrectomy with internal limiting membrane peeling versus inverted
internal limiting membrane flap technique for macular hole-induced retinal
detachment: a systematic review of literature and meta-analysis. BMC
Ophthalmol 2017;17(1):219.
https://doi.org/10.1186/s12886-017-0619-8
PMid:29179705 PMCid:PMC5704533
|
|
|
|
|
33 Zheng Y, Kang M, Wang H, Liu HY, Sun T, Sun
XD, Wang FH. Inverted internal limiting membrane insertion combined with air
tamponade in the treatment of macular hole retinal detachment in high myopia:
study protocol for a randomized controlled clinical trial. Trials
2018;19(1):469.
https://doi.org/10.1186/s13063-018-2833-y
PMid:30165894 PMCid:PMC6117933
|
|
|
|
|
34 Velez-Montoya R, Ramirez-Estudillo JA,
Sjoholm-Gomez de Liano C, Bejar-Cornejo F, Sanchez-Ramos J, Guerrero-Naranjo
JL, Morales-Canton V, Hernandez-Da Mota SE. Inverted ILM flap, free ILM flap
and conventional ILM peeling for large macular holes. Int J Retina Vitreous
2018;4:8.
https://doi.org/10.1186/s40942-018-0111-5
PMid:29479478 PMCid:PMC5817800
|
|
|
|